Allergic Conjunctivitis
Q: What are the causes of red eye?
A: The commonest causes of red eye are
- Infective conjunctivitis
- Allergic conjunctivitis
- Uveitis
- Acute angle closure glaucoma
- Dry Eyes
- Many many more……
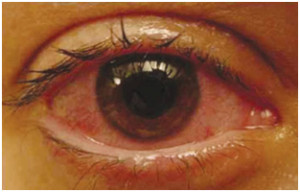
Q: What is allergic conjunctivitis?
A: Eye allergies are also called “allergic conjunctivitis.” It is a reaction to indoor and outdoor allergens (such as pollen, mold, dust mites or pet dander) that get into your eyes and cause inflammation of the conjunctiva, the tissue that lines the inside of the eyelid and helps keep your eyelid and eyeball moist. Eye allergies are not contagious.
Q: How common is allergic conjunctivitis?
A: 60 % of the general population have some form of allergy. The numbers are higher in metros and cities. 20 % of the general population have eye allergy. Approximately 4 percent of allergy sufferers have eye allergies as their primary allergy, often caused by many of the same triggers as indoor/outdoor allergies. For some, eye allergies can prove so uncomfortable and irritating that they interfere with job performance, impede leisure-time and sports activities, and curtail vacations.
Q: What causes eye allergies?
A: Allergens are what trigger your eye allergies. To the body, allergens are considered foreign substances that threaten or irritate the body, such as pollen from ragweed or cat dander. If you react to certain allergens, this means your eyes have become sensitized at some point. Therefore, when your eyes come into contact with specific allergens, an allergic response results.
Eye allergies are grouped in various ways, one of which is where the allergens are located—indoors or outdoors. Some allergens are more likely to be found indoors. Others you’re more likely to be exposed to outdoors.
INDOOR ALLERGENS Examples of common indoor allergens that may cause itchy eyes are airborne cat dander and dust mites.
OUTDOOR ALLERGENS Examples of common outdoor allergens that often trigger itchy eyes are grass, tree, and ragweed pollens.
Other substances called “irritants” (such as dirt and smoke, chlorine, etc.) and even viruses and bacteria, can compound the effect of eye allergies, or even cause irritation symptoms similar to eye allergies for people who aren’t even allergic. The eyes are an easy target for allergens and irritants because, like the skin, they are exposed and sensitive. Certain medications and cosmetics can also cause eye allergy symptoms. By way of response to these allergens and irritants, the body releases chemicals called histamines, which in turn produce inflammation.
Q: What are the signs of eye allergy?
A: The common symptoms of eye allergies are the result of this inflammation:
- Redness
- Itching
- Burning
- Tearing or watering
- Swollen eyes
- Gritty sensation in the eyes
- Intolerance to contact lenses
These symptoms may be accompanied by a runny or itchy nose, sneezing, coughing, or a sinus headache. Many also find that their vision is temporarily blurred, or that they feel distracted, unproductive, or tired.
Q: I have these symptoms all through the year? Can it still be allergic conjunctivitis?
A: There are two types of allergies.
- Seasonal allergic conjunctivitis: In this type eyes are affected only in a particular season. Summer, winter or wet season depending on the cause of allergy (allergen)
- Perennial allergic conjunctivitis: In this type eyes are affected throughout the year. This kind is similar to other severe forms of allergy like Bronchial Asthma. It is common in children. Also people having this form of allergy have some other severe allergic conditions like skin allergy (atopic dermatitis) or allergic bronchitis or Asthma.
So, allergy can recur throughout the year. However the eyes have to examined to rule out other causes of red eye especially uveitis.
Q: Can children have allergic conjunctivitis?
A: Yes. Infact allergic conjunctivitis is very common in children, similar to tonsillitis or adenoids. It commonly persists till about 15 years of age and then in majority of patients it subsides thankfully.
Since the course is chronic, children have to be treated carefully, making sure the side- effects of medication don’t damage the eyes. So self medication is not advisable, not just in children but even in adults.
Q: How are eye allergies treated?
A: The best defense against allergic conjunctivitis is to first avoid contact with substances that trigger your allergies. When prevention is not enough, consider over-the-counter or prescription treatments. Eye allergy symptoms may disappear completely, either when the allergen is removed or after the allergy is treated.
- Oral medication
Oral anti-histamines are crucial apart from eye medications. Till overall allergy is treated, ocular allergy is not going to subside completely.
- Eye medication
- Ocular medications like anti-histamines and NSAIDs help in controlling the ocular allergy to certain extent.
- Lubricants help in washing away the allergens and the toxic inflammatory material.
- In some severe cases, mild steroid eye drops are needed to treat the allergy.
Q: Can allergic conjunctivitis cause vision loss?
A: In majority of cases it does not cause vision loss. However in severe cases, it can cause corneal ulcers, which if untreated can cause vision loss.
Q: How to prevent allergy?
A: Eye allergy can be prevented by:
- Don’t touch or rub your eye(s).
- Wash hands often with soap and water.
- Wash your bed linens and pillowcases in hot water and detergent to reduce allergens.
- Avoid wearing eye makeup.
- Don’t share eye makeup.
- Never use another person’s contact lenses or misuse contact lenses
Q: Can contact lens cause allergy?
A: For contact lens wearers, eye allergies can cause unique problems. During allergy season, there are many loyal contact lens wearers who revert back to their eyeglasses due to discomfort. But many others develop strategies that allow for daily lens wear in comfort and ease. And as for those with allergies who think they cannot wear contact lenses – the fact is many of them can.
In the past, contact lens wearers have been interrupted by allergies, especially seasonal allergies, causing some to discontinue lens-usage, and others to stop considering contact lenses as an option. But some of today’s contact lenses are far more accommodating for people with allergy-related eye conditions. In addition, they are available in multiple modalities, including daily disposable and two-week replacement. Your doctor will direct you to the right lens for your vision and lifestyle needs. Replacement wear lenses require maintenance—cleaning and disinfecting every day after removal—as proteins, allergens, and lipids cling to their surface. These can cause discomfort, particularly for allergy-sufferers.
Smart Strategies for Contact Lens Wearers
Here are some strategies that doctors recommend:
- Limit wearing time.
- Make your own allergy-season “paradigm shift,” by wearing your lenses part-time, for example, for sports, social events (e.g., weddings and proms), and photos with family and friends.
- Use daily wear, two- or four-week replacement contacts.
- Use eye drops as prescribed by your doctor.
Studies have shown that single-use contact lenses can be a healthy option for contact wearers in general, including for some people with eye allergies.
Amblyopia (Lazy Eye)
Q: What is Amblyopia?
A: When a young child uses one eye predominantly and does not alternate between the two eyes, the prolonged suppression of the nondominant eye by the brain may develop into amblyopia. Amblyopia is sometimes referred to as “lazy eye,” but it is more than just an eye problem. The visual portion of the brain is suppressed and vision actually decreases in the unused eye.
There are different causes of amblyopia:
- Misalignment of the eyes with one eye not being used properly
- A need for glasses that has not been corrected
- Glasses are needed because one eye is out of focus
- The presence of a cataract (an opacity of the lens inside the eye) that distorts light images from properly focusing on the back of the eye, preventing good vision from developing for that eye
- A droopy or enlarged eyelid that covers the pupil and blocks the vision in that eye
In some cases there may be more than one cause.
Q: How is amblyopia treated?
A: Amblyopia (“lazy eye”) is by far the greatest cause of treatable vision loss in India. A child with amblyopia may lose vision in the affected eye permanently if the situation is not corrected early. Treatment is more difficult and less effective with children older than 9 or 10 years of age.
If your child is diagnosed with amblyopia, an individual active treatment program will be designed. This program may involve one or more of the following: eyeglasses, patch therapy, eye drops that dilate the pupil, and in some cases a contact lens. Your ophthalmologist will give you specific information about the treatment for your child.
Q: Won’t eyeglasses help?
A: In cases where child has high refractive error (high power glasses) and child has never used one, appropriate glasses can help the child see well. However glasses alone don’t help, other treatments have to be given to treat amblyopia.
Q: What about contact lenses?
A: In children who have a significant difference in the refractive error (power) between two eyes as a cause of amblyopia, contact lenses can be tried in the eye with higher error along with other amblyopia treatment.
However it needs proper hygiene and good child cooperation, which in most cases cannot be possible. Hence contact lenses are given only in select cases. Glasses are preferable.
Q: What is Occlusion (Patch) Therapy?
A: In order to improve your child’s vision, you may be instructed to patch an eye. Patching is a common method of treatment for the various types of amblyopia. This type of visual loss cannot be corrected by glasses alone or with surgery. The treatment is effective when it forces the child to use the “lazy eye” by patching the good eye. Patching is most effective in young children, but can also help improve vision in the early teen years. Untreated, amblyopia cannot be reversed, and the visual loss becomes permanent. Clear instructions, reasonable expectations, patience and consistency are all part of the comprehensive approach to your child’s eye care.
Q: How does my child adjust to the patch?
A: All children who are patching have similar problems. It is uncomfortable and sometimes difficult to adjust to wearing a patch. Your child may not see well at first, and this can be frightening. However, it does not hurt, and it does not damage your child’s normal eye. It is the best thing to do to preserve vision for a lifetime. For that reason, it is important that your child wear the patch as directed. (You will receive instructions on how often to patch your child.)
Q: Will the patching not damage the skin?
A: The patch must be of an adhesive type that sticks to the face. A “pirate patch” with strings or elastic is NOT advised. Be sure that the patch sticks firmly to the skin for the duration of patching time. The narrow end of the patch is placed toward the nose and the broad end away from the nose.
Patches come in regular and junior sizes and may be purchased at drug stores.
Although eye patches are hypoallergenic, some children develop mild skin irritation from wearing the patch. The broad area can be trimmed with scissors so that less adhesive contacts the face. The patch may be rotated slightly so that the same part of the skin is not always under the adhesive. To protect the skin and decrease irritation, you may apply Milk of Magnesia with a cotton ball to the skin area where the patch will stick and allow it to dry completely. Be careful not to get Milk of Magnesia into the eye. Then apply the eye patch as usual.
Q: How to remove the patch?
A: Removing an adhesive eye patch can be uncomfortable and distressing to the parent and child. Try to remove the patch slowly while applying pressure to adjacent skin to lessen pulling. Soaking the patch with cool water before removal is also helpful. Another method is to rub petroleum jelly or vaseline into the adhesive portion of the patch. Let the petroleum jelly soak in for about 30 minutes before gently pulling off the patch. The skin surrounding the patched eye can be treated with any skin care product to lessen skin irritation. Avoid getting any product into the eye.
Q: What to do if my child removes the patch?
A: If your child removes the patch before the full amount of time that he/she is supposed to wear it, immediately replace it with a new patch. Refocus your child’s attention with a toy or game in order to help to distract him or her from awareness of the patch. Be persistent. Since the patch is not painful, most children will wear the patch once they realize that their parents intend for them to wear it, and that it will be replaced. Young children can be discouraged from removing the patch by placing them in mittens or pediatric arm restraints.
Q: What to do after patching?
A: While your child is wearing the eye patch, he/she should be encouraged to use the other eye as much as possible. To shorten the patching period, encourage your child to participate in detailed busy work such as paint-by-numbers, connect-the-dot books, colouring, writing, drawing and tracing.
Some slight redness of the eye is common because children frequently rub the eye or the patch. Extreme redness, accompanied by discharge, should be reported immediately to your eye doctor. If at any time during the patching routine your child contracts measles, chicken pox, poison ivy, or any other type of skin eruption around the eye, DISCONTINUE the patching.
Q: What is the effect of the patch on the better eye?
A: If the cause of amblyopia is a squint, then sometimes the deviation seems to switch eyes or get worse with the patch. This is normal and only means that the “lazy eye” is now being used so that it stays straight while the other eye turns. This indicates that the patching program is having an effect. Improving vision in the weaker eye is the first step. The deviation can be dealt with when the lazy eye’s vision has recovered. Keeping return visits is important so any changes can be tracked.
Q: How long will my child need to wear the patch?
A: Patching will be continued until there is no further improvement in visual activity or until your child uses one eye equally as well as the other. It is impossible to predict how long this will be for each child, but it typically lasts for several months with some less intense patching thereafter. Patching could be one of the most important steps in the treatment of your child’s eye condition. Do not become discouraged! No matter how difficult it may seem, the long-term results are well worth it.
Q: What if my child must wear the patch while at school?
A: Some children will need to wear the patch at school or at the day care facility. If your child removes the patch frequently at home, this will probably also happen at school. Make sure your child’s teachers understand the importance of the patch. Provide them with extra patches so they can be replaced at school when needed.
Please help your older child to deal with the comments that others will make about the patch. Just as a leg plaster and crutches help while a broken bone is healing, the eye patch is a short-term way of helping your child to have better vision for life. Practice an answer to any questions that will satisfy the questioner and make your child feel positive about the process. For example, when asked “What is that on your eye?” the response could be “It’s a patch to make my weaker eye stronger.”
Q: What is Atropine Treatment for amblyopia?
A: Atropine drops may be used to treat your child’s amblyopia. Atropine blurs vision in the better-seeing eye and encourages use of the eye with poor vision and improves vision in that eye over time. Atropine may be used in addition to or as an alternative to traditional patching therapy. Because atropine cannot be removed once applied, it is a good treatment option.
Q: How to apply the drops?
A: Have your child lie down on his/her back, looking up at the ceiling. Hold the eyelids apart and let one drop fall anywhere between the eyelids. If the child is frightened, try giving the drop before he or she wakes up. In some children, it is necessary for one adult to hold the child while the other gives the drop. Eventually a routine will be established. Be sure to wash your hands after applying the drop so that you do not accidentally get any medication into your eyes. Also, take care not to get any of the drops in your child’s other eye.
Q: What to expect from the drops?
A: Unlike other types of eye drops, atropine usually does not sting. These drops cause the pupil (black center of the eye) to become very large. Your child may notice that close objects are blurred. This is the normal effect of the drops and may last for up to a week following one drop of atropine. Your child may also be bothered by bright sunlight. Sunglasses or a broad-brimmed hat may be worn outdoors on sunny days to avoid discomfort.
Since atropine blurs the vision of the better eye for near work, this forces the child to use the weaker eye for reading, drawing, etc. Allow your child to hold reading material close or to lean close to the desk. If your child attends school, please notify his/her teacher of the eye treatment. In some cases, reading glasses may be prescribed for using the better eye while at school.
Q: What are the side effects of atropine?
A: Rarely, a child may develop redness and swelling around the eye, fever, or a red warm face and neck. If this occurs, STOP using the drops and contact our clinic. Be sure to keep the atropine drops out of the reach of children. If a child drinks atropine from the bottle, contact your paediatrician immediately. It is an emergency.
Q: How long do I continue giving the drops?
A: Atropine treatment may be continued for weeks or months, depending on your child’s age and the severity of the vision loss in the amblyopic eye. Keep using the drops as instructed until the next appointment day unless your doctor says differently.
Q: Will my child’s vision improve with surgery?
A: Many patients who have amblyopia due to squint will eventually need an operation to align the eyes called squint surgery.
In cases of cataract or lid drooping, surgery is required to remove the cause of amblyopia followed by patching, glasses or both. Surgery alone will not improve your child’s vision.
Other causes of amblyopia will not require surgery.
Q: What is the prognosis?
A: Most cases of amblyopia do well if compliance with treatment is good. Majority of children will have good enough vision to do normal activities. However it ultimately depends on age of child, severity of amblyopia and presence or absence of other co-morbidity factors.
Age Related Macular Degeneration (ARMD/AMD)
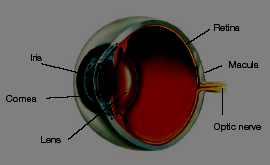
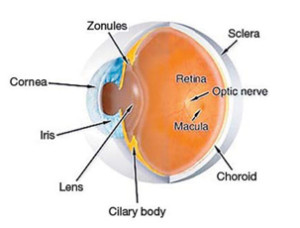
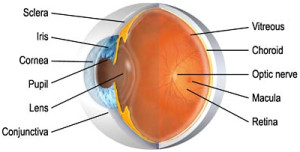
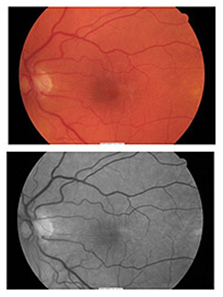
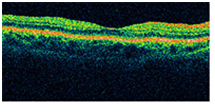
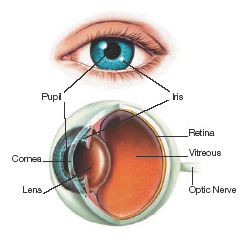
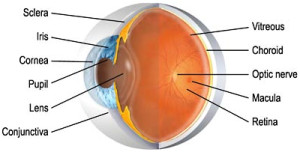
Q: How do we see?
A: Our eyes are like a camera with a lens system at the front of the eye, and the retina, like a photographic film, lining the inside wall of the back of the eye. Light passes through the cornea, pupil and lens and is focused on the light sensitive retina to form an image. Messages are sent via the optic nerve to the brain for processing.
Q: What is macula?
A: The macula is the central part of the retina. It is a small, specialized area in the middle of the retina and is responsible for our ability to see fine detail. This central vision is the vision we use for reading, driving, recognising faces, threading needles and other fine detailed work. The remaining part of the retina is responsible for our side vision, also known as peripheral vision.
This is our mobility vision, allowing us to get about and to maintain our independence.
Q: What is ARMD?
A: With ARMD, there is damage or breakdown of the macula, leading to loss of central vision. The eye still sees objects to the side since peripheral vision is not affected. For this reason macular degeneration does not result in total blindness.
Q: What is Dry ARMD?
A: The most common form of the disease is known as Dry ARMD. This form occurs in approximately 80 to 90% of people with ARMD.
Q: How severe is it? How does it affect my vision?
A: In Dry ARMD the vision loss is usually very gradual and is seldom severe. Areas of the central retina gradually become thin and stop working. Some people notice blank areas in their vision.
Q: How can I prevent or cure it?
A: Vitamin supplementation, diet modification and stopping smoking can all decrease the rate at which this gets worse, and the eyesight may also be helped somewhat with the use of special low-vision magnifying lenses.
Q: What is Wet ARMD?
A: Some people develop a more aggressive form of the disease called Wet ARMD that can lead to rapid and severe vision loss. This occurs in only 10 to 15% of people with macular degeneration. In Wet ARMD, abnormal blood vessels grow under the macula and eventually leak fluid, bleed or lift up the retina. When this happens central vision is reduced and often distorted. The longer these abnormal new vessels continue to leak, bleed and grow, the more central vision will be lost.
Q: Will I become blind?
A: Left untreated, these fragile vessels will cause scarring and irreversible loss of the detailed central vision. Sometimes only one eye loses vision while the other eye continues to see well for many years. If both eyes are affected however, reading and close-up work may become extremely difficult. It does not cause blindness and since the side vision remains, people can usually take care of themselves quite well.
Q: What are the symptoms of Macular Degeneration?
A: Most patients with ARMD will notice difficulty in reading as words become blurred or crowded. There may be a black or grey spot in your central vision. A frequent and important early symptom of Wet ARMD is distortion when straight lines appear bent or wavy. You may become aware of this when looking at a page of small print or looking at a window frame or telephone pole with your affected eye.
These changes in eyesight are important symptoms and if they occur you should contact your ophthalmologist promptly. Do not assume you simply need a new pair of glasses and wait for an appointment in the future.
Q: How is ARMD diagnosed?
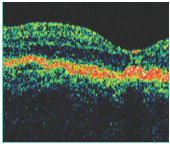
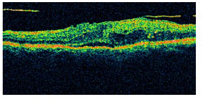
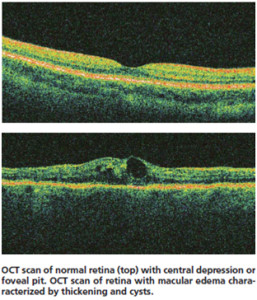
A: Many people do not realize they have macular problems until blurred vision becomes obvious. An eye specialist can examine the macula and identify early changes. If Wet ARMD is suspected, special tests called optical coherence tomography (OCT) and fluorescein angiogram are usually required.
OCT is a no-touch method of scanning the macula to look for fluid leaks, the first sign of Wet ARMD. It only takes a minute to do, and no needles or touching of the eye are required.
Fluorescein angiography is used to locate exactly where the leaking blood vessels are. In this test, dye is injected into a vein in the arm. The dye travels through the body, and with a special camera a series of photographs are taken as the dye passes through the retina, putting together a map of the problem which can be used by the doctor during treatment.
Q: What is the treatment for Dry ARMD?
A: With any kind of ARMD, various measures have been shown to decrease the risk of the disease getting worse. These include:
1. Vitamin Supplementation
A large American study, the Age-Related Eye Diseases Study (AREDS) found that using certain combinations of vitamins could reduce the chance of ARMD getting worse by about one quarter.
2. Stop smoking
Smokers are at higher risk of ARMD, and of Wet ARMD in particular. It is therefore very important to stop smoking at the earliest sign of this condition.
3.Dietary changes
Various foods seem to protect against the development of Wet ARMD, including nuts and fish oils.
Q: What is the treatment for Wet ARMD?
A: With Wet ARMD, several different treatments are possible:
1. Avastin/ Lucentis/ Macugen Injections
These drugs at present appear to be the best treatment for Wet ARMD. They are injected into the eye, and may need to be repeated several times over the course of several months, but they have been shown to improve vision in people with Wet ARMD, so long as scarring has not started to take place. No other treatment seems to improve vision; other treatments can only decrease the rate at which things get worse.
2.Thermal Laser Therapy (Photocoagulation)
In this procedure, the heat from a laser light is used to cauterize the abnormal leaky blood vessels. This treatment also damages overlying normal retina. This is done only if new blood vessels are away from the macula.
3. Photodynamic Therapy (PDT)
PDT uses a light-activated drug (Visudyne) and a special non-thermal laser to selectively destroy abnormal blood vessels while preserving surrounding normal healthy tissue. It is used less frequently now since the injections are proven better than PDT alone.
Q: Do the injections have any side effects?
A: Like any procedure on the body, these injections also have side effects which are thankfully rare.
With any injection in the eye, there is always a risk of infection or retinal detachment, the chances of which are 0.1 %. Occasional reports of excess reaction in the eye, increase in eye pressure, episodes of stroke and heart problems have been reported. Overall these drugs are safe, highly effective and are used worldwide.
Q: How do monitor my vision?
A: Amsler Grid Eye Exam can be used at home for monitoring one’s vision.
Directions:
- Wear the glasses or contacts you normally wear for reading.
- View the grid at reading distance (approx 30cm) in a well-lit room.
- Cover one eye with your hand and focus on the centre dot with your uncovered eye. Repeat with the other eye.
- If you see wavy, broken or distorted lines, or blurred or missing areas of vision you may be displaying symptoms of ARMD and should contact your eye care provider immediately
Q: Is there no alternative to repeated injections?
A: Unfortunately not till now. Research is on in this field. Many new drugs in the form of better injections and even eye drops are in the pipeline in the near future. In fact a drug called Eyelea is already available in Europe, which shows comparable results as Avastin and Lucentis, if not better. However it may take some time to reach Indian shores.
Cataract
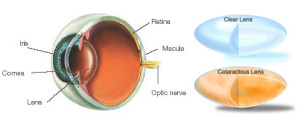
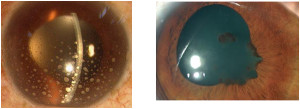
Q: What is cataract?
A: A cataract is an opacity (or cloudiness) in the lens of the eye. This cloudiness develops inside the lens and restricts light passing through the eye and reaching the retina. When this occurs,vision is affected.
An opacity can be quite minor or it can become so marked that it prevents adequate vision.
Q: What causes a cataract?
A: The most common cause of cataracts is aging. Others include:
- Inherited or developmental problems
- Health problems such as diabetes
- Medications such as steroids
- Trauma to the eye
Q: How will I know if I have a cataract?
A: People with cataract generally complain of the following-
- Cloudy or blurry vision
- Light sensitivity from car headlights that seem too bright at night; glare from lamps or very bright sunlight; or the appearance of a halo around lights
- Poor or reduced night vision
- Double or multiple vision (this symptom often goes away as the cataract progresses)
- “Second sight” where near vision becomes possible without glasses again because of the cataract developing in the lens. This state is usually temporary, and followed by progressive loss of distance vision
- A need for frequent changes of glasses or contact lenses
However only a doctor can tell you whether the above complaints are due to cataract only or something else. Other eye conditions, for example glaucoma, agerelated macular degeneration, injury and previous eye operations can also affect your eyesight.
Q: What is the treatment of cataract?
A: When a cataract is not fully formed, it may be possible to improve your eyesight with glasses. Your ophthalmologist will advise you if glasses are suitable.
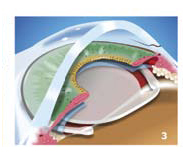
When the cataract grows too dense, glasses will not be effective and cataract surgery is necessary.This involves removing the cloudy lens from inside the eye through a small incision,and replacing it with a new artificial lens, alsocalled the Intraocular Lens (IOL) made from acrylic materials.
Q: What is an intraocular lens (IOL)?
A: It is an artificial lens, made from acrylic materials used to replace the natural lens and is implanted inside the eye during surgery.
They are broadly of two types.
- Monofocal lenses
They are the commonest types of lenses implanted in the eye since last 20-30 years. They can correct only distance vision. Glasses are required for near vision. However vision quality is very good. Monofocal lenses with Aspheric Optics (Premium Lens) results in clearer, brighter,better quality vision with enhanced contrast,most noticeable in low light conditions such as driving at dusk, in fog or drizzle, and with restaurant lighting. - Multifocal lenses
They are newer generation of lenses. They can give you both distance and near vision without glasses. However some patients may require glasses for both in spite of multifocal lenses due to variable healing response of the eye.They might give rise to glare at night especially for driving. Also vision quality in low light conditions can be affected. However with the newer lenses available, these problems occur rarely.Also not everyone can opt for multifocal lenses. There are some strict guidelines for using these lenses, which if not followed can give rise to the above problems and even more. You doctor can clarify these details with you if you need them.There are other special lenses like TORIC lenses which can be used in selected cases of high astigmatism. They require high level of expertise and generally give good results. However glasses may still be required after implanting them as well.Ultimately let your doctor decide what is best for you and which lens will suit your eye.
Q: When can one undergo cataract surgery?
A: In earlier times, cataract surgery was only done when the eyesight was very bad. Advances in technology mean that modern surgery is less traumatic to the eye. The results are more predictable, there are few side effects and the eye usually recovers quickly.Modern cataract surgery is done when people find their failing eyesight does not let them do their day today activities.
Q: Will I recover complete vision after cataract surgery?
A: Other eye conditions, for example glaucoma, age related macular degeneration, injury and previous eye operations can also affect your eyesight. Your ophthalmologist will examine your eye and advise you on the possible effects of other eye disease on the cataract surgery. In some cases eye condition scan affect the timing of surgery e.g. it may be better to delay surgery if active diabetic retinopathy is present and prepone it if corneal problems or glaucoma are present.
Q: How does one fix up cataract surgery?
A: At the consultation with your ophthalmologist, your operation can be booked within a few days. You will be checked about your medications, general health and drug allergies. Your ophthalmologist will discuss what focus you want after surgery. For example it may be possible to have your eyesight sharp for distant objects (sharp driving vision without glasses) or for near objects (sharp vision for reading without glasses). It may also be possible to have astigmatism corrected.
A laser or ultrasound machine is used to measure your eye. This gives data on the shape of the eye. From these figures, your ophthalmologist will choose appropriate lens implant to be used in your operation.
Your ophthalmologist’s staff will advise you the exact time & date of your operation.
Q: Is the surgery painful? Will I be made unconscious?
A: You will be asked to report one hour before the scheduled operation time. Drops will be put into the eye to dilate the pupil. Local anaesthetic is used to numb the eye. The local anaesthetic is given as an injection. In the operating theater you will be awake under a sheet. An instrument holds your eye open so you do not have to worry about blinking. The operation takes about 10-30 minutes. After the operation you may have a pad on your eye overnight. More detailed instructions will be given to you after your operation.
Q: What are the risks of surgery?
A: All surgery, no matter how technologically advanced, carries risk. Minor complications can lead to extra appointments or medications after the operation. In some cases, extra operations are needed. Complications can delay the recovery of your eyesight after surgery. Minor complications usually do not cause loss of eyesight. Serious complications such as infection and bleeding in the eye can cause loss of eyesight. Fortunately, serious complications are rare. Your surgeon will discuss with you the potential benefits versus the potential risks of cataract surgery.
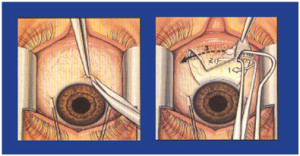
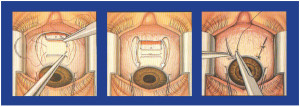
Q: What surgical technique is used?
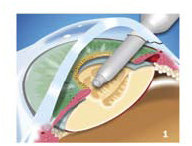
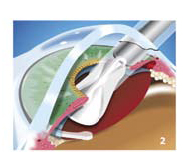
A: All surgeries are done with the latest “Phacoemulsification” technique through a very small 3 mm incision. It uses ultrasound power (misunderstood as LASER by general public). The steps are illustrated below.
Q: What are the precautions one has to take after surgery?
A: Surprisingly, there are no major restrictions nowadays after cataract surgery. Only one restriction is no head bath for a week after cataract surgery. Also one has to wear dark protective glasses to prevent discomfort from bright light and dust, but that also when one goes out of the house in the sun. At home, no such glasses are required. Also eye drops have to be applied for 3-4 weeks as necessary.
One can watch TV, do computer work, read papers or books, go for a walk from the same day of surgery. Ladies can do cooking etc also. No restrictions while sleeping also. For reading one can use the old glasses to read with the other eye. Any other doubts, feel free to ask your doctor.
Q: Will I require glasses after surgery?
A: Most of the times you will be able to most of your work without glasses. However, for fine distance and near work, glasses may be required. This differs from patient to patient. This is because the doctor is only human and cannot replicate nature’s precision.
Q: Is cataract surgery permanent?
A:Yes. It is not possible to get another cataract once it has been removed. However,approximately 10% of patients may become aware of a gradual blurring of vision some months or even years after the surgery due to thickening of the lens capsule that supports your artificial lens. If this occurs, clear vision is usually restored by a simple laser treatment,called a capsulotomy, which can be performed during a short visit to the clinic.
Eye problems in children

What are the common eye problems in children?
1. Refractive error (glasses) is commonest Amblyopia (Lazy eye)
2. Allergic Conjunctivitis
3. Squint
4. Cataract
How will I know if my child has glasses or no?
1. Child rubs his/her eyes
2. Goes close to the tv or holds things close
3. Does poorly/ not take interest at school and visual activities
4. Refuses to read/ study
5. Squinting of eyes
6. Headache and eye strain
7. Rarely child may complain of reduced vision
8. Rarely recurrent stye/ chalazion (boils on the lids)
What if my child has refractive error (glasses)?
1. Child just has to wear glasses as advised by your doctor
2. There is nothing wrong with the eye if the child has glasses
3. Plus powered glasses may go after some time
4. Minus powered glasses (distance glasses) are generally for life and may increase over time due to child’s growth
5. Watching too much TV/ mobile/ tablets etc do not give your child a refractive error or glasses
6. Refractive errors are hereditary or due to growth of the child
7. Refractive errors will stabilise once the childs growth is completed at around 18-21 years of age
What is amblyopia or lazy eye?
1. If both eyes have high power
2. If difference in the power between two eyes is more
3 If any or both eyes have a squint
4. If any of the above conditions not treated with appropriate glasses or surgery
Then,
a. The part of brain related to eye(s) does not develop
b. This causes blurred/ decreased vision in one or both eyes even though the eye is otherwise fine
Refer to ‘’Amblyopia’’ brochure for further details
Your child rubs his eye frequently and they become red. What to do?
 1. Your child could be having allergic conjunctivitis
1. Your child could be having allergic conjunctivitis
2. Quiet common in childhood like tonsils
3. Unfortunately recurrent till 12-15 years of age, then subsides on its own
4. Treated with medications under medical supervision
- In severe cases mild steroids are given to reduce severity of attack</li>

- Please do not self-medicate since the drugs can have side effects like
- cataract and glaucoma if misused
- In mild cases or recurrences, other anti-allergics are given, which are relatively safer
- Lubricants or tear substitutes are given to wash away the allergens (things that cause allergy)

- and toxic matter formed by the allergic reaction. They are very safe and can be used on a SOS basis
5. Rarely your child could be having a refractive error (glasses) also
Your child has a squint. What to do?
2. Some squints get corrected just by wearing appropriate glasses
3. Some squints are not significant and can be safely observed
4. Some squints require surgery especially if causing lazy eye
5. Your doctor is the best judge in such a condition
Refer to “Strabismus” brochure for further details
My child watches TV all day, plays mobile all day. Will it harm his eyes’’?
– God has given eyes to see
– Using them doesn’t harm them
– Excess of anything is bad
– She/he won’t get glasses due to this
Do eye exercises help? Will my child’s number or squint reduce with exercise ?
– They do not help in reducing your child’s number or squint
Does my child require any special diet like carrots, spinach etc?
– The normal balanced diet we give our children is sufficient
– Carrots, spinach etc are good but not of any special benefit for the eyes
Diabetes and Diabetic Retinopathy
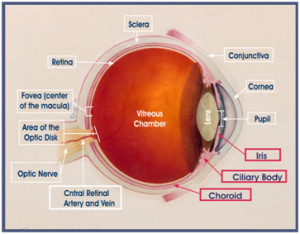
Q: What is vitreous?
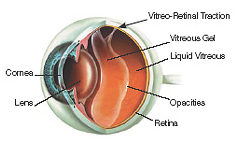
A: The eye is a ball of about 2.5cm diameter. The cornea and lens at the front of the eye focus light onto the retina (Figure 1). The eye is similar to a camera, with the focusing lenses in front, and the light sensitive film (retina) lining the back. The vitreous is the clear gel (jelly) which fills up the space inside the eyeball, behind the iris (the blue or brown part) and the lens.
Q: What is retina?
A: Retina lines the inside of the wall of the eye. The retina transforms light into electrical impulses, which travel up the optic nerve to the brain.
Q: What is macula?
A: The macula is the central part of the retina. It is a small, specialized area in the middle of the retina and is responsible for our ability to see fine detail. This central vision is the vision we use for reading, driving, recognising faces, threading needles and other fine detailed work. The remaining part of the retina is responsible for our side vision, also known as peripheral vision. This is our mobility vision, allowing us to get about and to maintain our independence.
Q: How do we see?
A: Our eyes are like a camera with a lens system at the front of the eye, and the retina, like a photographic film, lining the inside wall of the back of the eye. Light passes through the cornea, pupil and lens and is focused on the light sensitive retina to form an image. Messages are sent via the optic nerve to the brain for processing.
Q: How does diabetes affect the eye?
A: Diabetes can affect the eye in several ways. It can damage your sight by causing cataract, but also more importantly, by causing diabetic retinopathy.
Q: What is diabetic retinopathy?
A: Diabetic retinopathy is a potentially blinding complication of diabetes that affects up to a half of diabetics to some degree. At first you may notice no changes in your vision, but diabetic retinopathy can worsen over the years and damage your sight. With timely treatment, over 80% of people with advanced diabetic retinopathy can be prevented from going blind. We recommend every diabetic have an eye exam through dilated pupils at least every two years.
Both type 1 and type 2 diabetics are at risk of diabetic retinopathy. Pregnancy is a relatively high risk period for worsening of diabetic retinopathy and close follow up during pregnancy is recommended.
Q: How does diabetic retinopathy affect vision?
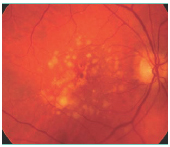
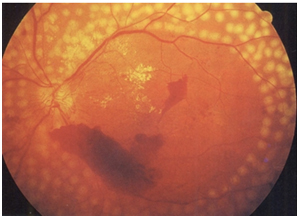
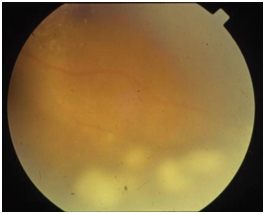
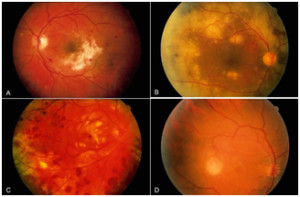
A: Diabetic retinopathy occurs when the small blood vessels in the retina become damaged by high blood sugar levels. It affects the eyes in two forms.
Macular oedema describes the condition where retinal blood vessels develop tiny leaks in the very centre of the retina. When this occurs, blood, fluid and lipids leak out causing swelling of the macula.
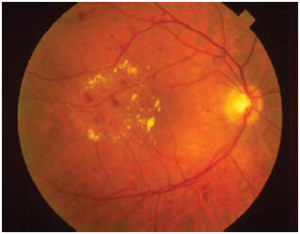
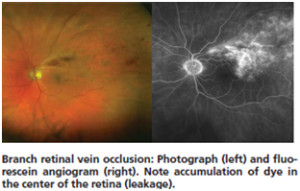
Small bleeds and areas of blood vessel leakage in an eye with macular oedema. Yellow deposits are lipid.
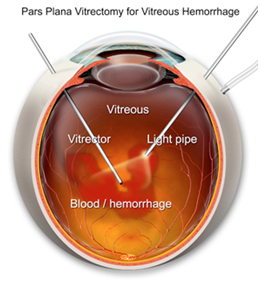
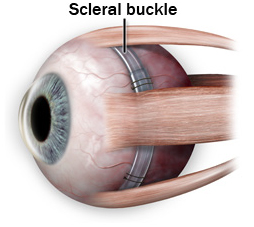
Proliferative diabetic retinopathy describes the changes that occur when abnormal blood vessels begin growing on the surface of the retina. These new blood vessels have a tendency to bleed or cause adjacent scar tissue growth. Leaking blood from these blood vessels can cloud the vitreous jelly that fills the centre of the eye and cause severe blurring. Scar tissue formation can lead to retinal detachment, which if left untreated often leads to blindness. If these abnormal blood vessels start growing around the pupil you can also develop a diabetic type of glaucoma, which can be very difficult to treat.
Q: What are the symptoms of diabetic retinopathy?
A: Many people with severe sight threatening diabetic retinopathy have no eye symptoms at all and therefore regular checks are required to allow treatment to be applied before it is too late.
The common symptoms are:
1) Blurred vision and difficulty reading
2) Sudden loss of vision in one eye
3) Dark spots floating around inside the eye
If you have these symptoms, it doesn’t mean you definitely have diabetic retinopathy, but you should have your eyes checked.
As part of your eye examination, you may occasionally be asked to have special imaging tests performed called OCT scans and fluorescein angiograms.
Q: How can I prevent diabetic retinopathy?
A: Unfortunately, one cannot prevent diabetic retinopathy. It is a progressive disease. Having regular eye checks every 1 to 2 years is the most important thing you can do. Good blood sugar control and blood pressure control also reduce the risk of developing advanced diabetic retinopathy. Regular physical exercise is important to control diabetes and diabetic retinopathy.
Q: What is the treatment of diabetic retinopathy?
A: In most early cases of diabetic retinopathy, treatment is not required, but ongoing observation is still needed. When required, it can be any of the 3 means, depending on the type and stage of retinopathy.
Laser surgery is the mainstay of diabetic retinopathy treatment. It is done for both macular oedema and Proliferative diabetic retinopathy. Proliferative diabetic retinopathy requires up to 3 sittings of laser on 3 different (could be consecutive) days. This is usually a clinic procedure that means you don’t need to go to the operating theater. The laser is applied through a contact lens system. During the procedure you will see bright lights in your vision. For the rest of the day your vision may be blurred and the eye may feel a little bruised.
Laser treatment has its limitations. The main aim of laser is to maintain existing vision and prevent further vision loss. Occasionally bleeding can happen following the procedure, in proliferative diabetic retinopathy due to the disease itself and not due to laser.
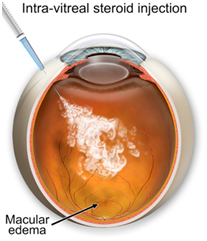
Injections into the eye of various drugs are required to stabilize diabetic retinopathy mainly macular oedema. This sometimes has to be repeated and may be required in conjunction with laser treatment or vitrectomy surgery. Presently, injections with laser are the preferred treatment option for macular oedema, with results better than laser alone.
Vitrectomy surgery is occasionally performed on eyes with advanced diabetic eye disease. If you have a lot of blood in the vitreous jelly, removal of the jelly with a vitrectomy will clear away the cloudiness in your vision. Sometimes this surgery is also performed if you have a retinal detachment associated with your diabetic retinopathy. A vitrectomy is usually a local anaesthetic procedure, which means you will be awake at the time, with the eye fully numbed.
Q: What are the injections to be given in the eye? Are they painful? What are the risks?
A: Currently we have three options in injections.
1. Treatment with Lucentis or (Accentrix in India)(Ranibizumab)
There is a new treatment that is effective in improving vision and clearing macular edema in diabetic retinopathy. It is injection of Lucentis into the eye once a month for at least six months. Lucentis is an antibody against the molecule that causes macular edema and the growth of abnormal vessels (Vascular Endothelial Growth Factor or VEGF)
Vision improvement is rapid and seen on average, by seven days. Patients are treated with three to six monthly injections. After six months it may be possible to stop the treatment, but this varies from patient to patient. If the vision is down, we usually restart treatment immediately. If vision is good and there is no macular edema, observation may be continued.
2. Treatment with Avastin (Bevacizumab)
This is another Anti –VEGF drug, which is FDA approved for treatment of cancers and has also been shown to work for macular edema. Research has proven it to be equally effective and safe as Lucentis.
We prefer to use Lucentis when possible and patient permitting, because it is the drug that has been shown to work in large clinical trials and is prepared under strict and specific FDA guidelines for use inside the eye.
3. Treatment with Steroids
They are used only in diabetic macular edema.
Intraocular steroid injections like triamcinolone (IVTA) and Ozurdex are another treatment option. The duration of action is much longer and so the need for less frequent injections. In some cases like persistent macular edema, they are more effective than anti-VEGF injections.
However there is a significantly higher risk of glaucoma and cataracts in patients given steroid injections, especially if they are repeated.
Ozurdex is a long acting steroid implant, which contains a different steroid, dexamethasone. The duration of action is for about 4 months. The risk of cataract and glaucoma is marginally less than triamcinolone (IVTA).
While Lucentis is a better, safer option for most cases, sometimes steroid treatment by itself or in combination with Lucentis may be warranted.
Both Avastin and Lucentis are used in diabetic macular edema as well as in proliferative diabetic retinopathy, especially prior to surgery.
All the above injections are given under topical anaesthesia. So they don’t cause any pain. All the injections have a risk of eye infection and retinal detachment. Thankfully these are very rare. The additional risks with steroid injections are mentioned above.
Q: What is end result of diabetic retinopathy?
A: Patients who have milder disease and have got treatment at appropriate time end up having moderate to good vision. Patients with advanced disease, in spite of treatment have moderate to poor vision depending on the blood supply to the retina and macula and health of the retina.
Epiretinal Membrane
Q: What is Retina?
A: The retina is a thin delicate tissue that lines the inside of the back of the eye. It is nerve tissue that senses light that shines into the eye, converts the light into an electrical signal and sends this signal through the optic nerve to the brain, which then processes the information resulting in sight. The macula is the very central area of the retina that gives us sharp central vision and reading vision, as well as most of our colour vision.
Q: What is an epiretinal membrane?
A: An epiretinal membrane is a thin sheet of fibrous tissue that can develop on the surface of the macula. When a membrane develops on this very thin, delicate macular area of the retina it acts like a film through which it is harder to see than normal. Furthermore, it may contract just as scar tissue does, pulling on the retina and distorting it, causing not only distortion of the vision due to distortion of the macula, but also causing the retina to become swollen and work less well. Because it is often the distortion of the macula that is the most obvious feature of this problem, it is sometimes also called a macular pucker, premacular fibrosis, surface wrinkling retinopathy or cellophane maculopathy.
Q: What causes an epiretinal membrane?
A: In most cases an epiretinal membrane is idiopathic, that is it develops in an eye with no history of any previous problems. It is not due to anything the afflicted individual has done, but instead is caused by natural changes in the vitreous gel overlying the macula that cause normal biological cells derived from the retina and other tissues within the eye to become liberated into the vitreous gel and eventually settles onto the surface of the macula. In some cases these cells may begin to proliferate into a “membrane”.
In many instances this membrane remains very mild and does not have any significant effect on the macula or the person’s vision. In other cases however, the membrane may slowly become more prominent, eventually creating a disturbance in the retina that leads to visual blurring and/or distortion in the affected eye, particularly if the membrane contracts.
However, an epiretinal membrane can also develop if cells are liberated into the eye by a previous problem, such as a retinal tear or detachment, trauma, inflammatory disease, blood vessel abnormalities, or other conditions. These are called secondary epiretinal membranes; they have the same effect on vision as the idiopathic type and are treated in the same way.
Q: How does an epiretinal membrane affect vision?
A: Many epiretinal membrane are mild and have little or no effect on vision. However, if the epiretinal membrane grows more prominent and contracts, causing mechanical distortion (“wrinkling”) of the macula , blurring and/or distortion of the central portion of vision in the affected eye may occur and may get slowly worse over time.
An epiretinal membrane does not make an eye go completely blind. It typically affects only the central area of vision and does not cause a loss of the peripheral (side) vision.
Q: Is an epiretinal membrane the same as macular degeneration?
A: No! An epiretinal membrane and macular degeneration are completely different conditions affecting the retina
Q: Is there treatment for an epiretinal membrane?
A: Yes. An epiretinal membrane can be treated with surgery. However, not all epiretinal membranes require treatment. Treatment is unnecessary if the epiretinal membrane is mild, stable and having little or no effect on vision. Only cases in which the membrane is causing problems require consideration of surgery. However, it an epiretinal membrane is getting worse it is better to remove it sooner rather than later, as severe mechanical distortion of the macula may cause permanent changes that removing the membrane may not improve or only improve to a limited extent.
There is no other treatment apart from surgery for an epiretinal membrane.
Q: What is epiretinal membrane surgery like?
A: The surgery for a epiretinal membrane is called a vitrectomy. This surgery is usually done as a day (outpatient) surgery using a local anesthesia, and takes up to an hour. The surgery consists of making very small ports through the white part of the eye (the sclera) 3 mm behind the edge of the cornea. Newer surgical techniques and instrumentation allow the surgeon to perform the surgery through tiny “self-sealing” incisions that do not require sutures. This new technique allows faster healing of the eye with minimal or no post- operative ocular irritation.
While looking into the eye through a microscope the surgeon can use a variety of very specialized instruments placed through these incisions to work within the eye. The vitreous gel is first removed as is the posterior hyaloid membrane which is at the back of this gel. This holds the gel together like the skin of a balloon filled up with water; removing it also removes any floaters that one may have. The vitreous gel is then replaced with a specially designed saline solution. The surgeon can then “peel” the epiretinal membrane from the surface of the macula. Sometimes the surgeon also peels a very thin membrane (the “internal limiting membrane of the retina”) from the surface of the macula which can become puckered by the epiretinal membrane sitting on top of it. Steroid treatment or air are commonly placed inside the eye to hasten the rate at which the retina recovers from having been distorted by the membrane, and laser and freezing (cryotherapy) treatment is usually also used to secure the peripheral retina in place.
Q: What is the postoperative care like after epiretinal membrane surgery?
A: A patch is worn over the eye until the morning after surgery. Eye drops (an anti-inflammatory and an antibiotic) are then used several times each day for up to 4 weeks after surgery. Patients can usually resume normal non-strenuous physical activities the day after surgery. How quickly the patient can drive, return to work, perform fine visual tasks, or engage in strenuous activities will vary from person to person.
Q: How much will my vision improve after surgery?
A: The amount of visual improvement will vary depending on the age and anatomic characteristics of the epiretinal membrane, how significantly the vision has become affected by the epiretinal membrane, and the presence of any other ocular abnormalities that might limit vision. It is not unusual to recover vision of 6/6 or 6/9 after successful epiretinal membrane surgery, and the distortion improves in 90% of patients. However, some individuals may have more limited improvement in vision, especially if the membrane had been there for a long time and the vision had already become very poor, and a small percentage of people may not improve very much at all even with successful surgery. It takes anywhere from 3 months to 1 year for vision in the affected eye to reach it’s maximal improvement.
Q: What complications may occur as a result of epiretinal membrane surgery?
A: Any surgical procedure carries a risk of complications and this surgery is no exception. There are 3 major potential complications of surgery:
1. Post-operative infection (endophthalmitis): This is an infection that develops inside the eye after ocular surgery. Though most infections can be effectively treated if identified at an early stage, there is a risk that an infection can create severe damage that could lead to blindness in the affected eye. Fortunately, endophthalmitis is rare, occurring in only 1 of 1000 cases.
2. Retinal detachment: Retinal detachment can occur spontaneously in an eye that has never had surgery of any type. However, an eye that has undergone surgery is at greater risk of developing retinal detachment. A retinal detachment may occur relatively soon after surgery, but may occasionally develop months or years later, and can lead to blindness if not repaired. Fortunately nearly all retinal detachments can be between 1 and 2 out of 100 cases.
3. Cataract: Cataracts, or haziness in the lens of the eye, commonly develop as a natural consequence of aging of the eye. However, a cataract will often develop or progress to a point of significant visual blurring sufficient to warrant cataract surgery more quickly after having had this surgery. This is not a concern if the patient has had cataract surgery prior to having a vitrectomy surgery.
Glaucoma
Q: How do we see?
A: The visual system is like a digital camera (the eye) connected to a computer (the brain) that makes sense of what the camera detects. The optic nerve is the “cable” that connects the eye to the brain. Nerve fibres carry visual messages from all parts of the retina, which lines the eye and detects light and colour. These nerve fibres come together at the optic disc to form the optic nerve.
Q: What is glaucoma?
A: Glaucoma is a common eye condition (or group of conditions) that can lead to blindness – in fact glaucoma is the second most common cause of blindness around the world. Fortunately if glaucoma is detected early and managed appropriately in nearly every case blindness is preventable. Glaucoma is most often controlled with eye-drops, but laser, tablets and surgery are also used in its treatment.
Glaucoma is a disease of the optic nerve, the “telephone cable” that carries visual information
from the eye, where images are captured, to the brain, the computer that makes sense of what is seen. Most cases of glaucoma proceed very slowly as optic nerve fibers are gradually lost.
Q: What causes glaucoma?
A: Intraocular pressure (IOP) (pressure inside the eye) normally ranges between 10 and 20 mm of Hg. Rise in this intraocular pressure reduces the blood circulation to the optic nerve and damages it. Other causes of reduced blood supply to the optic nerve including age, hypertension (raised blood pressure), diabetes mellitus, hyperlipedemia (raised cholesterol), heart disease, smoking and drinking can contribute to glaucoma.
Q: Who can get glaucoma?
A: Babies, children and young adults can get glaucoma, but these types of glaucoma are rare. Glaucoma becomes much more common as we get older, occurring in 2% of the population over 40 but in as much as 11% of the population over 80. As mentioned above people having other illnesses have a higher risk of developing glaucoma. Glaucoma may also follow on from other eye disease or eye injury. People with a family history of glaucoma have a higher risk of developing glaucoma.
Q: What are the types of glaucoma?
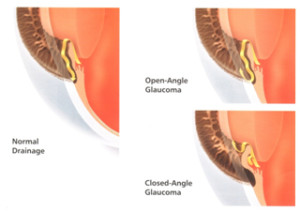
A: There are many different types of glaucoma. The two main types of glaucoma are Primary Open Angle Glaucoma (POAG) and Closed Angle Glaucoma (CAG).
Q: What is Open angle glaucoma?
A: Most people with glaucoma have forms of POAG. There is most often a family history. There is damage to the drainage system of the eye, leading to increase in IOP, leading to glaucoma.
Q: What is closed angle glaucoma?
A: The second most common type of glaucoma is Primary Angle Closure Glaucoma (PACG). There is narrowing of the drainage passage in the eye due to smaller eyeball size (as in people having high plus number) or due to thickening of lens due to cataract. This can develop very slowly, like open angle glaucoma, or can occur suddenly in the case of Acute Angle Closure Glaucoma, where the eye becomes very red and painful and vision is lost in a matter of days if appropriate treatment is not begun.
This form of glaucoma is more common in Indians/ Asians than western people due to relatively smaller eyes.
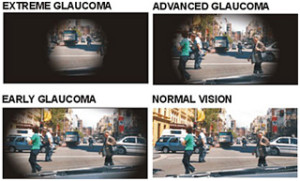
Q: What will be my complaints if I have glaucoma?
A: Unfortunately the brain does not recognise that patches of vision are missing until the damage from glaucoma is very advanced, so sufferers of glaucoma will only be aware they have a problem very late in the disease. It is for this reason that it is of the utmost importance that we all have regular eye examinations from the age of 45, earlier if we have glaucoma in the family. People go blind because they have glaucoma but haven’t realised this, often for many years.
Only in the closed angle type of glaucoma will a person have complaints. Patients will complaint of pain, redness, cloudy vision, coloured rings around lights, severe headache or even vomiting.
Q: How will I know if I have glaucoma?
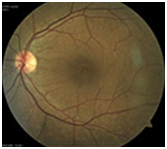
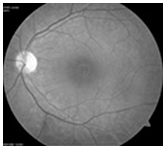
A: Normally with glaucoma there is no perceived visual disturbance nor eye discomfort to warn that someone has glaucoma. Glaucoma is detected through routine eye examinations by your ophthalmologist. Glaucoma is often associated with elevated eye pressure, and discovery of this may be how your glaucoma is detected. Glaucoma causes a characteristic type of erosion of the optic disc we call cupping, which can be seen when the back of your eye is examined.
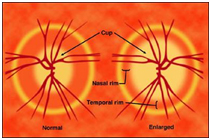
Drawings of a normal disc (left) with a normal sized cup, then a disc with ‘cupping’,enlargement of the cup due to loss of nerve tissue from glaucoma
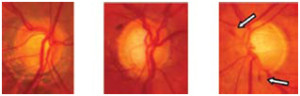
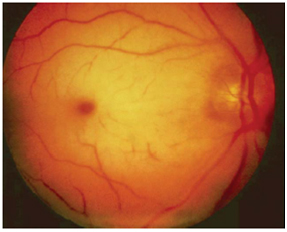
Photos of cupped discs: in the third disc small disc haemorrhages also typical of glaucoma can be seen
Q: What is visual field testing?
A: Glaucoma causes loss of visual field, patches of one’s vision. This is detected by visual field
testing. Monitoring the visual field is particularly important to ensure that glaucoma is controlled
and not getting worse – most people with glaucoma will have field tests once a year.
Q: How to manage glaucoma?
A: Your ophthalmologist will assess and then usually treat your glaucoma. As well as asking about past eye problems and your general health, and examining your eye, your ophthalmologist will establish your glaucoma diagnosis and a treatment plan doing some or all of the following:
- establish at what level your eye pressures are running
- ensure he has a reliable, repeatable record of your visual fields
- measure your corneal thickness (pachymetry)
- record your optic disc appearance with stereo photos
- measure your nerve fibre layer thickness with the OCT
Management of glaucoma is all about detecting that glaucoma is present or not. It can take up to a year to confirm whether a patient has glaucoma or not. Till then a patient is treated as a glaucoma suspect.
This is followed by monitoring the patient to detect whether the disease is controlled, or that more damage is occurring. This is done in several ways. It is important to examine the patient’s optic discs for further cupping or disc haemorrhages which are indications of progressive glaucoma. For many discs however only big changes can be detected.
Visual field testing is another important way to monitor glaucoma, but field loss occurs relatively late in the disease, and even good subjects will have variable field results depending on how tired they are, and how well they can concentrate on this demanding test.
Q: What is OCT?
A: The OCT is a relatively new, very sophisticated machine that can actually measure the thickness of the nerve fibre layer at the back of the eye, down to microns (thousandths of a millimeter). We can compare an individual’s OCT result to normal references, and in particular, to the individual’s test results from previous years, to see if change has occurred. For the patient the test is simple and painless, rather like having a photograph taken. It is however still a supporting test for visual fields, which is still the gold standard.
Q: What is the treatment of glaucoma?
A: At present the only way we can treat glaucoma is by lowering eye pressure. If we get the eye pressure down to a safe level, in almost all cases of glaucoma we will halt the disease, or at least slow it down so that significant vision impairment does not occur in the patient’s lifetime. The level of pressure that is safe is different for each patient, so we set “target pressures” for each individual. (Generally speaking, the lower the eye pressures the better).
1. Eye drops: Most glaucoma patients instill eye drops to keep their eye pressures at a safe level. A patient may be on one, two or more different glaucoma eye drops. These medications are for lifetime or as instructed by your ophthalmologist.
2. Laser treatment
a. Laser trabeculoplasty is a very safe and generally painless way to treat glaucoma and should be considered for all newly diagnosed cases of glaucoma. Successful laser treatment can keep the eye pressure down for a few years without requiring eye drops. Eventually patients end up applying eye drops. (The laser used is very different from the laser used to allow people to manage without glasses.)
b. Laser peripheral iridectomy is a safe and painless way of trying to prevent angle closure glaucoma in patients at risk for the same. However it is still a temporary measure as compared to early cataract surgery.
c. Laser iridoplasty is to treat patients with plateau iris syndrome (a form of narrow angle glaucoma)
3. Surgery (trabeculectomy) is also used to treat glaucoma: it is employed when the eye pressure cannot be controlled by drops and laser, and when patients cannot tolerate eye drops (or manage to get them in regularly) or in advanced glaucoma. It is rarely done nowadays.
4. Early Cataract Surgery is recommended in patients with narrow angles or chronic angle closure glaucoma, since it permanently opens up the angle and also reduces the IOP to some extent.
5. Combined cataract and glaucoma surgery is done in certain cases as required.
6. End stage Glaucoma where in patient does not much vision and pressure is not controlled with medications, a special form of laser called Diode Cyclophotocoagulation is done to keep eye pressures down. Also Anterior Retinal Cryopexy (ARC) may be required under local anaesthesia for neovascular glaucomas (glaucomas caused due to diabetes/vein occlusions).
7. Repeated injections in the eye may be required before laser or ARC can be done to prevent neovascular glaucoma.
8. Enucleation (removal of the eyeball) may be rarely required in painful blind eyes due to glaucoma.
Blood pressure, diabetes and lipid (cholesterol) control, regular exercise, avoiding smoking and tobacco and improving overall health also helps control glaucoma.
Q: What is the course of glaucoma?
A: Having glaucoma means that you must have a life-long association with your ophthalmologist. The disease can be controlled but not cured, and it is essential that patients are seen regularly (for most this is six monthly). Typically glaucoma is well controlled for a number of years but then at a follow-up visit it is found that control has been lost, for instance that the visual field is worse, and that a change in treatment is necessary. It is the ophthalmologist’s, and the patient’s responsibility to make sure that patients do not become “lost to follow-up”.
Macular Hole
Q: What is retina?
A: The retina is a thin delicate tissue that lines the inside of the back of the eye. It is nerve tissue that senses light that shines into the eye, converts the light into an electrical signal and sends this signal through the optic nerve to the brain, which then processes the information resulting in sight.
Q: What is macula?
A: The macula is the very central area of the retina that gives us sharp central vision and reading vision, as well as most of our colour vision. The fovea, the central area of the macula, is the thinnest and most fragile section of the retina.
Q: What is a Macular Hole?
A: A macular hole is a defect in the macular area, which is the central area of the retina. It is in the foveal area that a macular hole can develop. If a macular hole does develop, this small tear or hole then expands with time, letting fluid pass under the retina, causing enlargement of the blur. This process eventually becomes stable, but seldom improves without treatment. A macular hole does not lead to total loss of vision, but usually does lead to legal blindness in the affected eye if untreated.
Q: What causes a macular hole?
A: The most common cause of a macular hole is an anatomical change occurring spontaneously between the clear vitreous gel of the eye, and the macula, creating a small tear or hole in this delicate area of the retina (which expands over time).
These are naturally occurring changes, not caused by the individual and anything they have done (or neglected to do). For a small percentage of people, these natural changes become pathological, resulting in mechanical stresses in the macula that may cause a hole to form. Generally called an idiopathic macular hole, this kind of hole is most common in individuals over 50 years of age.
On the odd occasion, an eye subjected to severe blunt trauma can develop a macular hole. A very small percentage of people with retinal detachment are also affected by a macular hole, as are some conditions that cause severe edema (swelling) of the retina. These types of macular holes occur mostly in people under 50 years of age, are not widespread, and can be differentiated without difficulty from the more common idiopathic macular hole.
Q: How is a Macular Hole treated?
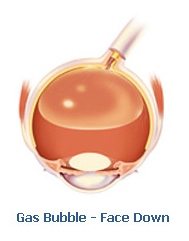
A: Surgery is the only treatment available, with a success rate of 90-95%. Vitrectomy is a procedure where the majority of the vitreous gel is removed from the eye. A large gas bubble is placed in the eye, flattening the edge of the macular hole. This bubble goes away by itself after several weeks. For 90-95% of patients, this process will lead to the macular hole disappearing. 85% will experience vision improvement, if the hole does disappear.
As with any surgery, it does not work for every patient, with the most likely aspects that predict success being the size of the hole, duration of symptoms, and original vision quality. Depending on vision prior to surgery, 60-85% will achieve driver’s license level of vision after surgery. Your Eye Doctor will discuss your personal situation and prognosis with you. In general terms the earlier the macular hole is detected and treated, the better the odds of success.
Q: How does a macular hole affect vision?
A: A macular hole affects the central element of vision, resulting in a loss of sharp, directly-in-front vision, and reading vision, in the affected eye. In the early stages, when the hole is small, vision is usually only slightly blurred or distorted. Vision progressively gets worse over a number of weeks or months, as the hole enlarges. Generally, the hole enlarges to the stage where the affected eye can only see the larger letters of a visual acuity chart. A macular hole does not bring about complete blindness as it affects only the very centre of vision, therefore not resulting in any loss of the peripheral (side) vision.
Q: Are macular holes and macular degeneration the same?
A: No – macular degeneration and macular holes are entirely different conditions, but both do affect the retina.
Q: What is macular hole surgery like?
A: Surgery to treat a macular hole is called a vitrectomy. This is usually a day-stay (outpatient) procedure performed at our centre, using local anaesthesia, and taking approximately one to two hours.
An operating microscope is used to see the retina and other structures inside the eye, and tiny incisions (under a millimeter in length) are made in the sclera (the white of the eye). Special instruments are then inserted through the incisions into the vitreous cavity to work within the eye.
Vitreous gel is removed from the eye, and replaced with a clear saline solution – such fluid comprises 99% of the natural vitreous fluid. The surgeon then typically peels a very thin membrane from the surface of the macula surrounding the macular hole.
Lastly, a gas bubble that completely fills the vitreous cavity is inserted to replace the saline solution. This synthetic gas is absorbed over time and replaced with the eye’s natural fluid called aqueous. A laser and freezing treatment is usually also used to secure the peripheral retina in place. Stitches are not normally required.
Our Center offers state-of-the art facilities for day stay eye surgery. You’ll enjoy quicker recovery and less disruption to your everyday activities.
Q: What is the post-operative care like after macular hole surgery?
A: A patch must be worn over the eye until the morning after surgery, and eye drops that facilitate healing are then used several times each day for 4 weeks. If possible, we ask people to position face down for five days immediately following the operation, but don’t worry if you can’t. The face down position permits the gas bubble to press firmly against the macular hole, which may increase the chance of the hole closing well, although the success rate is already 90 to 95% without doing this.
Q: After surgery, what improvements can I expect to my vision?
A: The extent of visual improvement will vary, depending on the macular hole successfully closing, the age and anatomic characteristics of the macular hole, and any other ocular abnormalities that might affect vision.
Most patients recover vision of 6/6 or 6/9 after successful macular hole surgery; however, some have more limited progress in vision improvement, and a small number of individuals may not improve much at all, even with successful surgery. Your Doctor will discuss in more depth about what you can expect and the possible outcomes with you, prior to surgery.
Q: When can I expect to see results?
A: It can take between 3 months and 1 year for vision in the affected eye to improve to it’s utmost potential. Patients who have had a macular hole for less than a year or two are much more likely to have an improvement in vision after this surgery. Those who have a macular hole for longer are less likely to notice an improvement.
Q: What are the possible complications of macular hole surgery?
A: As with any surgical procedure, there are risks of complications and macular hole surgery is no exception. Although the risks are very low, the three main potential complications of macular hole surgery are:
- Retinal detachment: Although retinal detachment can occur suddenly in an eye that has never had surgery of any type. After surgery however, an eye is at greater risk of developing retinal detachment. A retinal detachment can happen a short time after surgery, but occasionally develops months or years later, and if not repaired, can lead to blindness. Fortunately, nearly all retinal detachments can be repaired with surgery, and the frequency of retinal detachment after macular hole surgery is between 1 and 2 out of every 100 cases.
- Post-operative infection (endophthalmitis): This infection can develop inside the eye after any ocular surgery, causing damage that could lead to blindness in the affected eye. Fortunately, most infections can be successfully treated if recognized at an early stage, and having endophthalmitis is actually quite rare, occurring in only 1 out of every 1000 cases.
- Cataract: Cataracts (haziness in the lens of the eye) generally develop as a natural consequence of aging. However, an existing cataract can develop or progress to a point of considerable visual blurring after surgery, enough to justify cataract surgery in most eyes within a year of having a vitrectomy. This is not the case if the patient has already had cataract surgery before having a vitrectomy surgery.
Posterior Vitreous Detachment and Retinal Detachment
Q: What is vitreous?
A: The eye is a ball of about 2.5cm diameter. The cornea and lens at the front of the eye focus light onto the retina (Figure 1). The eye is similar to a camera, with the focusing lenses in front, and the light sensitive film (retina) lining the back. The vitreous is the clear gel (jelly) which fills up the space inside the eyeball, behind the iris (the blue or brown part) and the lens.
Q: What is retina?
A: Retina lines the inside of the wall of the eye. The retina transforms light into electrical impulses, which travel up the optic nerve to the brain.
Q: What is Posterior Vitreous Detachment (PVD)?
A: This occurs with age changes in the clear vitreous gel. Parts of the gel become liquid, pushing the remains of the gel forward, a condition called posterior vitreous detachment.
Q: What are floaters?
A: At the time of PVD, opacities frequently form at the liquid-gel interface. These are seen as floaters.
Q: Are floaters something to worry about? Will they reduce my vision?
A: They are common, and harmless in themselves. They don’t reduce your vision. However, with this degeneration in the vitreous, there is sometimes associated pulling on the retina, as in places the vitreous is adherent to the retina.
Q: What are flashes?
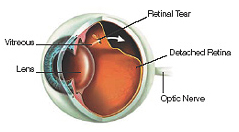
A: Pulling on the retina causes the sensation of flashes. You can see them even when the eyes are closed and more on moving the eye.If this pulling is severe enough, a hole or tear may occur in the retina. Then liquid vitreous may pass through the hole, peeling the retina off the back wall of the eye, which is a retinal detachment.
Q: What to do if you have floaters and/or flashes?
A:
- If you have had occasional floaters for years, don’t worry. The chance of retinal detachment is small.
- If you suddenly notice floaters, or experience at sudden increase in floaters, you should have your eyes examined promptly. This examination is to search for any retinal tears.
- If you develop flashing lights, seen usually at night, again you should have your eyes examined promptly. Flashing lights mean pulling on the retina and the risk of detachment is significant. However there are other possible causes of flashes, one of which is migraine. Nevertheless the sudden onset of flashes demands prompt examination of the retina. Floaters and flashes are warning symptoms which demand prompt examination, but most people who experience them never develop a retinal detachment.
Q: What is retinal detachment?
A: A retinal detachment occurs when the retina peels off the inside of the back wall of the eye. When detached, the retina does not function, so that when part of the retina is detached there is a gap in the vision and when the whole retina is detached the eye is blind.
Q: Who is at risk of retinal detachment?
A: Retinal detachment occurs in about 0.01% of the population. Although anyone can experience a retinal detachment, people with certain eye conditions are at increased risk. Some examples of these conditions include lattice degeneration, myopia (short sightedness), injury to the eye, complicated cataract surgery, etc..
Q: What are signs and symptoms of retinal detachment?
A: A retinal detachment is a medical emergency. Retinal detachment itself causes a sudden loss of part or all of the vision in the eye. It does not cause any pain. In many cases, as explained, a retinal detachment is preceded by floaters and flashing lights.
Q: What if my retina shows tears or holes?
A: If a tear is found before a retinal detachment occurs, laser or cryotherapy can be used to weld down the tear and reduce the chance of a later retinal detachment. However a few retinal tears are better left, a decision which needs to be made by your eye specialist. Treatment of retinal tears causes little or no discomfort and is performed as an outpatient procedure. During laser surgery tiny burns are made around the hole to “weld” the retina back into place. Cryopexy is a similar procedure that freezes the area around the hole.
Q: What is treatment for retinal detachment?
A: All retinal detachments are different, and the characteristics of the detachment determine the type of surgery. In most cases the surgery is done under local anaesthetic, although general anaesthesia may be preferable in certain circumstances.
Q: What is Pneumatic Retinopexy?
A: This technique is reserved for the least complicated detachments. A gas bubble is injected into the vitreous. It prevents liquid from travelling through the retinal tear and thus the retina re-attaches. At the same time or later, either laser or cryotherapy is used to seal the retinal tear to the back wall of the eye. It is necessary to stay in a particular posture for a few days afterwards to keep the bubble in the correct position.
Q: What is Scleral Buckling?
A: A piece of silicone is sutured onto the wall of the eye to counteract the force pulling the retina out of place. This is often combined with draining fluid from inside the eye and with injecting gas.
Q: What is vitrectomy?
A: The vitreous gel, which is pulling on the retina, is removed from the eye. This is usually combined with injection of gas or silicone oil, and often also with a scleral buckle. This combined technique is often reserved for more complicated detachments.
Q: What are the dos and don’ts after surgery?
A: There is usually some discomfort after surgery. If gas or oil has been inserted, then it may be necessary to assume a particular head position for 3 weeks. Air travel is unwise with a gas bubble in the eye, as the bubble may expand and cause a dangerous rise in the eye pressure. If oil is inserted another small procedure needs to be done after at least 4-6 months to remove the oil.
Q: What are the results of surgery? What about my vision?
A: If the retina can be successfully re-attached, the vision improves. However if the centre of the retina has been detached, the vision may never return fully. The sooner surgery is carried out the better, so it is important to see an eye specialist as soon as you suspect any trouble. Some patients, however, will need more than one procedure to repair the damage.
Strabismus
Q: How do eyes work?
A: The two eyes are coordinated by a central area in the brain and move together in a way that is similar to the front wheels of a car. One wheel cannot be moved without the other one moving. Likewise, you cannot move your left eye independently of the right eye. If one of your car wheels is bent inward, you can, by turning the steering wheel, make it straight. However, the previously straight wheel will now be turned in. The same concept of movement applies to the eyes. Thus, while it may appear that the right or the left eye is misaligned, it is really a problem between the two eyes. An eye muscle problem may be corrected by operating on either eye or, more commonly, on both eyes.

Like the steering wheel controls the front wheels of a car, the brain coordinates normal eye movement
Q: What is strabismus (squint)?
A: Strabismus is the medical term for misalignment of the eyes. It is a Latin word meaning “to look askance or sideways.” It refers to the problem of the eyes not working together and one eye turning in, out, up or down. Approximately four percent of children in India are affected by strabismus. There are various reasons for this condition, ranging from a need for glasses to ocular (eye) or neurological abnormalities. A parent or close relative is often the first to notice a vision problem. When a vision problem is suspected, a complete eye examination should be arranged as soon as possible. Early detection and management are important for best results.
Q: How is strabismus managed?
A: We assess visual acuity in infants and children, measure ocular deviations, and evaluate eye movements. The level of the examination will be adapted to your child’s ability to respond. We obtain much useful information through observation of your child’s visual behavior. Although responses are helpful, verbal ability is not necessary to complete an accurate eye examination.
Q: Will glasses help my child?
A: Some children have an inward turning eye (crossed eye) that is due strictly to farsightedness (accommodative esotropia). They must use extra focusing power to see clearly. Without glasses, one or both eyes turn in. Corrective lenses relax this extra focusing power so that the eyes stay straight. Glasses with or without bifocals are the best solution.
Children who have an occasional outward drift of one eye when tired may benefit from glasses with ‘minus’ power that help them to keep their eyes straight.
Glasses may be needed to provide clear vision and eliminate blurring, squinting, or abnormal head positions.
Q: Does a turned eye cause double vision?
A: When a child’s eyes do not work together as a team, he/she will look at an object with one eye while the other eye looks at something else. The image from the wandering eye causes double vision. But the brain, by a technique called suppression, switches off the wandering eye. Thus, younger children rarely have double vision.
Older children and adults with newly acquired eye muscle problems often report double vision. Sometimes double vision may be treated with the use of prisms that adhere to or are incorporated into a pair of glasses.
Q: Will eye exercises help?
A: Eyestrain and fatigue when reading may indicate a convergence problem. Measurements by us can determine if your child will benefit from eye exercises. Simple near-point exercises can be done even with young children.
Q: What can happen if I leave the squint untreated?
A: When a young child uses one eye predominately and does not alternate between the two eyes, the prolonged suppression of the nondominant eye by the brain may develop into amblyopia. Amblyopia is sometimes referred to as “lazy eye,” but it is more than just an eye problem. The visual portion of the brain is suppressed and vision actually decreases in the unused eye.
So an untreated squint can cause amblyopia and vice versa. Normally amblyopia associated with squint require hand in hand treatment of both squint and amblyopia.
Refer to our amblyopia brochure for further detail.
Q: I don’t have squint all the time. I have it occasionally. Do I need treatment?
A: This type of squint is called Intermittent Squint. It generally occurs at the end of the day, when you are tired or when you fall sick.
They are normally outward deviations (one eye going out). And this squint is common in adults who have been having it since childhood. Because it is intermittent, they have ignored it. It also leads to chronic eye strain due to the effort required to keep the eyes straight.
This type of squint may be partly managed with glasses and eye exercises. However in most cases, a time comes when the control of squint becomes poor and it starts occurring more frequently and may become permanent.
Surgical intervention is recommended when the control becomes poor and squinting becomes frequent.
Q: What is strabismus surgery?
A: Many patients with eye deviations will eventually need an operation to align the eyes. The goals of surgery are twofold. The first is to change the present eye alignment in such a way as to enable the brain to use both eyes together. This may re-establish binocular function. The second is to improve the appearance so that the eyes look straight and move together. The chances for achieving these goals are influenced by the size and complexity of the eye deviation, the age of onset, types of previous treatment, quality of binocular function (depth perception), and the compliance with pre- and post-operative therapy.
The results of strabismus surgery are not always perfect because human tissue varies from individual to individual. Therefore, it may take more than one operation to achieve the goal of straight eyes. The success rate varies from 50 to 90 percent, depending on the type of operation and condition of the eyes. In some cases the surgery may be performed in steps, with the first operation designed to correct only part of the problem. A second or even third operation may be necessary to deal with any residual misalignment or to correct another aspect of the problem. Sometimes the correction of one problem will uncover a second problem that was not apparent before the surgery.
The purpose of this discussion is to acquaint you with the facts about strabismus surgery. With vigorous and complete treatment the results are usually extremely gratifying.
Q: How the eye muscles work?
A: Eye muscle surgery involves either weakening or strengthening the muscles that control eye movement. There are six muscles that attach to the outside surface of the eyeball and control the movement of each eye. Four of these muscles are called rectus muscles and their functions are very straightforward. The superior rectus muscle attaches to the top of the eye and pulls the eye up. The inferior rectus muscle attaches to the bottom part of the eye and pulls the eye down. The medial rectus muscle attaches to the side of the eye closest to the nose and pulls the eye in. The lateral rectus muscle attaches to the outside of the eye closest to the ear and pulls the eye out.
Two additional muscles (the oblique muscles) have very complex eye movement functions. The superior oblique muscle attaches to the top back part of the eye and runs through a pulley near the top part of the nose. This muscle pulls the eye down when the eye is looking toward the nose. The inferior oblique muscle attaches to the bottom back part of the eye and pulls the eye up when it is looking toward the nose. Their primary function is torsion, the inward and outward rotational balance of each eye.
Q: What are the surgical procedures?
A: Strabismus surgery consists of two general types of operations. One is a weakening procedure of the muscle which is called a recession, and the other is a strengthening procedure which is called a resection. The technique for doing these operations is as follows: the eye muscle is reached through a small cut through the conjunctiva, which is a thin whitish skin over the surface of the eyeball. The conjunctiva is the part of the eye that gets red and bloodshot when the eyes are irritated. The eye muscles are immediately beneath this conjunctival tissue. Incisions through the skin of the face or the eyelids are not necessary to reach the eye muscles.
A common misconception is that the eye is removed from its bony cradle called the orbit and placed on the face during the operation. This is not true. The eye muscles are located approximately 1/4 of an inch from where the clear dome (called the cornea) meets the white tissue of the eye (called the sclera or conjunctiva). Therefore, it is not difficult to get to the eye muscles while the eye remains in its usual position.
Stitches used during surgery are later absorbed. There are no stitches that have to be removed at a later date. The distance that the muscles will be moved is normally determined before the surgery. The technique takes a great deal of skill to move the muscles correctly and is best performed by a doctor who specializes in this type of surgery. The time estimated for the actual surgery is about 20 minutes per muscle. It does not include the time necessary for falling asleep and waking up.
Q: Will the surgery be painful? What about anesthesia?
A: One of the risks of strabismus surgery is undergoing anesthesia. With today’s techniques and equipment, this risk is extremely small. The risk of a serious complication in a healthy child is approximately 1 in 500,000. It is safer in the operating room having a strabismus operation than it is riding in a car on a four-lane highway.
Every effort is made to ensure that the patient is in the best physical condition before he/she undergoes anesthesia. Prior to surgery you may be asked to obtain certain blood tests and X-rays as necessary.
The anesthetic concerns for strabismus surgery are different from most other types of surgery. Most patients are healthy, the operation is usually short, and major body systems are not involved. Potential anesthetic problems are minimized.
The surgery is most often done as an outpatient procedure. This reflects the relative safety and ease of recovery from general anesthesia used for eye surgery. Since eye surgery is “elective,” any condition that would increase the risk of complications from anesthesia must be eliminated prior to surgery. This is especially important in children. Conditions such as ear ache, pneumonia, flu-like symptoms, or GI problems will result in postponement of the surgery until they have been treated. It is safer to delay the surgery than to operate on a child or an adult who is sick.
Q: What are the complications of surgery?
A: During surgery every effort is made to reduce the likelihood of problems. However, during the course of any surgical procedure problems may arise. It is the surgeon’s responsibility to minimize these problems in the operating room. After the surgery, it is the patient’s (or parent’s) responsibility to follow carefully the instructions and treatment prescribed. The most frequently encountered complications are as follows:
- Overcorrection/undercorrection: This is not really a complication but is instead an undesirable outcome. Overcorrection or undercorrection of a misalignment may occur in the eyes being repaired. An overcorrection would be to make an eye turn out that previously turned in. An undercorrection would be an improvement in the alignment of the eyes but the eyes are still turned in. This failure to achieve optimal alignment occurs anywhere from 20–40 percent of the time and may result in the need for the use of glasses, special eye drops, prisms, or an additional surgical procedure.
- Infection: Infection may occur in the immediate post-operative period, but fortunately this is extremely rare. The ocular tissues are highly vascular and this usually aids in the prevention of this problem. You will be given instructions with regard to the use of antibiotics and in the care and use of the eyes in the immediate post-operative period. A post-operative visit will be scheduled to detect any early signs of an infection. Severe infection inside the eyes can result in loss of vision. Fortunately, this is very unusual after strabismus surgery.
- Bleeding/Retinal detachment: A small bleed into the eye may occur which normally resolves without intervention. Rarely (approximately one out of 10,000) a retinal detachment can result which will require further surgery to repair.
- Slipped muscle: The suture used to attach the eye muscle to the eye is extremely strong. However, in a rare situation the suture may break, which can cause the muscle to slip or become detached from the globe. This requires immediate surgery to reattach the muscle. Fortunately, this also rarely happens.
- Loss of vision: Permanent loss of vision from eye muscle surgery occurs approximately in one out of 10,000 eye muscle operations, or less. The cause is usually internal eye infection (endophthalmitis), internal eye hemorrhage, or retinal detachment. Early detection and treatment can save vision.
- Double vision: In the immediate post-operative period it is not unusual for the patient to see double (called diplopia). The eye muscles are sore and are not working correctly, or occasionally the eye position has been changed enough so that the brain processes two images instead of one. The double vision normally resolves within days to weeks, and in some cases it is desirable immediately after the surgery. Persistent double vision, however, may require additional intervention if it does not resolve in an appropriate period of time. Every effort is made to try to anticipate whether this will occur so that you or your child can be prepared in the immediate post-operative period.
- Change in refraction: Changes in eyeglass prescriptions may be necessary after eye muscle surgery due to slight alterations in the shape of the eye or cornea. This may not be permanent and new glasses will usually correct any refractive changes.
Q: What is the post-operative care?
A: Instructions for post-operative care will be given at the time of the surgery. Eyes vary in appearance and comfort depending on the type of operation and how much surgery was done. You can expect the eyes to be somewhat sore and irritated for at least several weeks after the operation. The conjunctiva will be red and swollen, and it may feel like you have sand or other foreign objects in the eye. Sometimes the upper and/or lower lids will retain fluid and swell. This usually resolves within several days. If both eyes are operated on, neither eye will be patched. If, however, just one eye is operated on, a patch will often be used to increase comfort.
It is recommended that most people remain out of work or school for a few days to one week following the surgery. While you may be able to resume your activities within a day or two, it is better to plan for a longer recovery period in case it is needed.
The two basic rules that should guide activities for the first week after surgery are:
- Nothing gets in the eye(s)—including rubbing eye(s) with your hands
- Avoid any possible injury to the eye(s)
If you apply these two rules to the planned activity and neither is an issue, then the activity is okay. Otherwise, DON’T DO IT! Questions about additional issues not covered here may arise. Please feel free to contact your doctor prior to surgery in order to get these questions answered.
Uveitis
Q: What is Uvea?
A: Uvea is the middle layer of the eye. It is the most vascular structure of the eye. It provides nutrition to the other parts of the eye. The uvea is made up of the iris (coloured part of the eye), the ciliary body (ring of muscle behind the iris) and the choroid (layer of tissue that supports the retina).
Q: What is uveitis?
A: Uveitis is inflammation (reaction in) of the uvea. Inflammation of the uvea usually causes a red eye, sometimes with cloudy vision, and it may be painful. Uveitis may be caused by an injury, infection or underlying disease. If it is not treated, the eyesight can be seriously damaged.
Q: Who is affected?
A: Uveitis can affect anyone. It particularly affects people of working age but can also occur in children.
Q: Are there different types of uveitis?
A: The type of uveitis depends on which part of the eye is affected:
- Anterior uveitis: This is inflammation of the front part of the eye i.e. iris (iritis) or inflammation of the iris and the ciliary body (iridocyclitis). It is the most common type of uveitis, accounting for 75% of cases.
- Intermediate uveitis: This affects the middle part of the eye i.e. area behind the ciliary body. It tends to occur in childen, teenagers and young adults. However adults can also be affected.
- Posterior uveitis: This affects the area at the back of the eye, the choroid and the retina.
- Pan uveitis: This affects all the three parts of uvea or the entire uvea.
Q: What is acute and chronic, which the doctor tells me?
A: Acute uveitis lasts for a few weeks and can recur, whereas chronic uveitis lasts for more than three months, with symptoms that can vary from day to day.
Q: How do I know if I have uveitis?
A: If you have uveitis, you will have some or all of the following symptoms.
- Anterior uveitis (iritis)
Anterior uveitis affects the front of the eye (usually the iris) and is the most common type. Only one eye is usually affected. Symptoms include:
- an aching, painful, red eye. The pain can range from mild aching to intense discomfort,
- blurred or cloudy vision,
- an iris (the coloured part of the eye) that may have a slightly different colour,
- sensitivity to light (photophobia),
- floaters (dots that move across the field of vision), and
- headaches.
These symptoms may develop gradually over hours or days. They may be acute (lasting a few weeks) or chronic (lasting for more than three months).
- Intermediate uveitis
Intermediate uveitis is the second most common type, affecting the area just behind the ciliary body and part of the retina. Both eyes tend to be affected and it is usually painless.
Symptoms can include:
- mild redness (although there is usually no redness),
- floaters (dots that move across the field of vision), and
- blurred vision due to cells from the blood vessels leaking into the gel of the eye.
There is usually no redness or only mild redness associated with intermediate uveitis.
- Posterior uveitis
Posterior uveitis affects the back of the eye (the choroid) where your blood vessels supply the retina. One or both eyes may be affected and it is usually painless.
Posterior uveitis usually causes decreased vision and floaters, and sometimes retinal detachment. These symptoms are slower to develop and often last longer than those of anterior uveitis.
Posterior uveitis can be more damaging to the eye than other types of uveitis. It sometimes causes visual loss.
Q: What is the cause of uveitis?
A: In about 50 % of the cases, we are unable to pinpoint a cause. But it may result from:
- an injury to the eye (traumatic iritis), for example, a squash ball hitting the eye,
- recent or previous eye surgery,
- certain types of infection, or
- a health condition (see below).
Health conditions
Uveitis may be associated with the following conditions:
- an inflammatory or autoimmune condition (when the body attacks its own organs), such as arthritis, juvenile rheumatoid arthritis, ankylosing spondylitis (arthritis of the spine), Reiter’s syndrome, Behçet’s disease, sarcoidosis, psoriasis or inflammatory bowel disease,
- a bacterial, viral, fungal or parasitic infection such as toxoplasmosis, gastroenteritis, tuberculosis (TB), Lyme disease, syphilis or shingles, and
- an immune-deficiency disease (when the body’s immune system is impaired), such as HIV/AIDS, because this can make you prone to infection.
Q: Your eye doctor tells you probably have tuberculosis, even when you don’t have any complaints of tuberculosis?
A: In our developing country, tuberculosis is presumed to be one of the most common causes of uveitis. You may not have any cough and chest involvement. But that does not rule out tuberculosis. You can have only ocular involvement. Some other part of the body could also be involved, which could be picked up on whole body scanning (which is impractical, unless you have other symptoms)
The only way to confirm ocular tuberculosis is taking a sample from you eye for histopathological evaluation, which is not possible in most cases. Hence the doctor has to go by clinical judgment and by your other test reports.
Q: How can uveitis be diagnosed?
A: Your ophthalmologist (eye specialist) will be able to diagnose uveitis based on your symptoms.
- If you have anterior uveitis, the most common type, one of your eyes will be painful and red.
- If you have one of the other, less common types of uveitis, your eye will usually not be painful.
Examination
- The eye is examined with a slit lamp (a microscope designed for eye examination). White blood cells and protein in the eye fluid can be seen through the microscope if you have uveitis. As the light beam passes through the eye, the fluid inside is seen to be hazy instead of clear.
- A light will be shone into the unaffected eye and this will cause both pupils to constrict. If one eye is affected by uveitis, there will be a slight pain in the eye as the pupil constricts.
- There will normally be an examination of the inside of the eye to see if other parts of the eye are affected.
- Uveitis must be distinguished from conjunctivitis. Conjunctivitis never affects vision (although it may cause clouding of vision if pus briefly gets onto the cornea) and it does not affect the inside of the eye, just the outside.
Q: Why did my doctor advise so many expensive blood tests?
A: Blood tests, X-rays and other tests are done to establish the cause of the uveitis. In 50 % cases tests turn out to be normal. These are the cases in which we are unable to find a cause. In such cases an auto immune cause is presumed and treated empirically (just treat the complaints, not the cause). Also before starting treatment, we need to be sure that there is nothing else wrong in the body, which can worsen with our treatment.
Q: How is uveitis treated?
A: Treatment of uveitis will depend on the type of uveitis, how serious it is and the cause. Some cases will clear up with the use of eyedrops. Others may need steroid injections into the eye.
The aim of treatment is to:
- control the inflammation,
- relieve any pain,
- treat any underlying condition, and
- treat any complications that may cause visual loss.
If you have recurrent uveitis, it is important to get it treated quickly. You may be advised to keep steroid eyedrops to hand at all times.
Q: What are the treatment options?
A: The different treatments are outlined below.
- Mydriatic eyedrops
- Mydriatic eye drops, such as atropine, homatropine or cyclopentolate, dilate (widen) the pupil. This helps the eye to heal, prevents the pupil from getting stuck to the lens and decreases the eye pain. Your doctor will advise how often you should use these.
- Mydriatic eye drops may cause blurred vision, difficulty focusing and an increased sensitivity to light, but they are a vital part of treatment.
- If the condition is diagnosed early and treated with eye drops, no visual loss should occur.
- Steroid eyedrops
- Steroid eyedrops help decrease the inflammation of the iris. They will be used frequently at first and then tapered off, to prevent the uveitis recurring.
- Steroid eyedrops may not used if a virus or bacteria caused the condition.
- Since the eyedrops do not go deep into the eye, they are generally used for anterior uveitis or panuveitis only.
- Steroid injections in the eye
- For intermediate and posterior uveitis, steroid injections are given directly inside the eye. The injection is done under local anaesthetic and you can go home on the same day.
- They can sometimes cause increase in eye pressure, retinal detachment or infection in the eye.
- However they do not have any side effects on the body. Hence preferred in patients in whom there is no contra-indication to steroid injections and steroid tablets are contra-indicated like diabetics.
- In some cases of anterior uveitis, steroid injections are given around the eye, which reduces the need to apply frequent steroid eye drops. It is painless and is done under local anaesthetic.
- Steroid tablets (such as prednisolone)
- Steroid tablets are given in intermediate or posterior uveitis.
- They have the advantage of acting on the causative condition in the body also. However they have side effects in the body.
- Intravenous Methyl Prednisolone
- In some very severe cases, a high dose steroid drip (methylprednisolone) may be given in hospital.
- Immunosuppressants
- Immunosuppressants are drugs that suppress the body’s immune system. Examples are:
- cyclosporine,
- azathioprine, and
- methotrexate
These tablets can be used alongside steroids to treat uveitis in severe and recurrent cases. They take some time to start acting in the body, hence steroid tablets are given as cover for early course of disease, till immune suppressants take over. They are also used in patients in whom steroids have caused lot of side effects or in whom steroid tablets cannot be given like diabetics, patients with CSR etc.
Also immune suppressants like steroids have their range of side effects. They too need to be monitored regularly.
Q: Won’t the steroid drops, injections or tablets harm me?
A: Yes, they do if not taken under medical supervision. All the above long term treatment have quite a few side-effects on the body and eye. Regular monitoring of side effects as advised by your eye doctor is advisable.
Most of the side effects of steroid tablets like weight gain, excessive hunger, acne, weakening of bones, mood swings etc are reversible on stopping treatment.
Q: What are the complications of uveitis?
A: Uveitis needs to be closely monitored because complications may develop and lead to loss of vision. Possible complications are outlined below.
- Raised eye pressure and glaucoma
- Untreated uveitis can cause the iris to stick to the front surface of the lens. This prevents fluid draining through the pupil and increases pressure inside the eye. It can lead to visual loss and glaucoma (damage to the optic nerve).
- Raised eye pressure can also be a side effect of steroid eye drops, so it is important to use the lowest possible dose of these.
- Cataracts
- Untreated uveitis can cause cataracts (cloudiness in your lens that can lead to visual loss).
- Prolonged steroid medication also causes cataract.
- Macular oedema
- Macular oedema is fluid that collects in a part of the retina called the macula. It can result from untreated posterior uveitis and may lead to loss of vision.
All the complications can be managed by either medications or surgery as advised by your eye doctor.
Q: Will my eye recover completely or will I lose my vision?
A: Uveitis should improve within two to three weeks of treatment. Traumatic uveitis (injury to the eye) usually goes away within a week.
The sooner treatment is started, the quicker the recovery. The length of treatment will depend on the severity of the condition and how the eye responds to treatment.
Follow-up appointments with an ophthalmologist (eye disease specialist) are essential.
Q: I had a similar episode of uveitis few months back. Why and what to do?
A: This is called recurrent uveitis. If your uveitis is associated with a disease, it may recur. If symptoms of a new episode are recognised quickly, prompt treatment will usually prevent the attack becoming severe.
If a treatable cause of uveitis is found and treated, uveitis will not recur. Otherwise most often than not, uveitis is recurrent depending on the disease. The frequency and duration of recurrence depends on the severity of attack, regularity in treatment etc. Timely intervention can prevent permanent damage to the eye. Recurrent cases generally require immunosuppressive.
Retinal Vascular Occlusions
Q: What is retina?
A: The eye is a spherical structure with the lens of the eye that focuses light in the front. In the back of the eye is the retina, which converts the images on the retina into electrical impulses and sends them along the optic nerve to the brain.
The retina has both arteries and veins (blood vessels). In most patients, there is a single artery or vein that enters the eye through the optic nerve. These are called the central retinal artery and central retinal vein.
These arteries and veins spread out to the periphery of the retina and the arteries and veins cross each other. These crossing points can cause problems as you get older because if the arteries become thickened, they can compress the vein.
Q: What are Retinal Vascular Occlusions (RVOs)?
A: A retinal vascular occlusion is blockage of the retinal vessels, either the arteries or the veins, in the back of the eye. If these blockages took place in the brain they would be called a “stroke”. As a result, we often call these problems “stroke in the eye”.
These blockages have different causes usually relating to a systemic disease like hypertension (blood pressure), diabetes mellitus, dyslipidemia (cholesterol problem), homocystinemia, anaemia, renal failure, liver problems, autoimmune disorders etc. and habits like smoking, tobacco and alcoholism.
Q: How do Retinal Vein Occlusions cause loss of vision?
A: Retinal Vein Occlusions cause vision loss in the following two ways
- Macula edema
The major cause of vision loss in retinal vein occlusion is macular edema. The macula is the central retina and is responsible for fine detail vision for reading, recognising faces and driving. It is an intricate and delicate structure that needs to have proper connections and needs to be free of swelling with fluid (edema).
In retinal vein occlusion, the blockage of the veins results in leakage of fluid and blood through the blood vessel walls. This is much like what happens when a garden hose is plugged and water leaks through the wall of the hose due to the increased pressure and damage to the rubber wall.
We are able to diagnose and monitor this complication with a test called Optical Coherence Tomography (OCT) scan. The OCT scan provides a cross section of the macula to evaluate its thickness and structure. In a normal OCT scan, the central macula has a thickness of between 150 and 250 microns (one fourth of a millimetre). A central depression call the fovea is what gives one the fine detailed 6/6 vision.
In macular edema, fluid accumulates and causes the macula to swell like a sponge. As a result, vision can be distorted or blurred, and the images may be magnified or minified much as when looking through a glass of water.
2. Neovascularisation and vitreous haemorrhage
This normally occurs around 3 months after the initial blockage if necessary treatment is not taken and in some cases in spite of treatment. The lack of blood supply to the area where the blood vessel is blocked, causes the retina to release many chemicals (VEGF etc.). These chemicals cause the formation of new, abnormal blood vessels, supposedly to supply blood to the affected area. These abnormal blood vessels are very fragile and can bleed on trivial jerks like coughing, sneezing, rubbing etc., causing bleeding inside the eye called vitreous haemorrhage.
This generally indicates poor prognosis and if left untreated causes rise in intraocular pressure (neovascular glaucoma) and painful blind eye.
Q: What are Central Retinal Vein Occlusion (CRVO) and Hemi-Central Vein Occlusion (HCRVO)?
A: A blockage of the main vein in the eye is called a central retinal vein occlusion. The blockage of the vein takes place in the optic nerve behind the retina. Because the blockage takes place outside the eye in the optic nerve, it usually affects the entire eye and vision may be severely affected.
In some patients there are two or more central retinal veins. These patients can have occlusion of only one of these veins and have what is called hemi-central vein occlusion. These often cause less damage than a full central vein occlusion.
Most patients who have this problem have risk factors for vascular disease. This may be diabetes, high blood pressure, arteriosclerosis, open angle glaucoma or a condition called thrombophilia. In younger patients, usually under age 40, we check for clotting disorders. We may find an important abnormality that needs to be treated. If there is a family history of strokes or miscarriages or if the patient has autoimmune problems, then the tests are particularly important. Since these problems are stroke-type events, we request that you check with your primary care doctor for a review of your medical condition.
The blockage causes blood to back up in the eye, which causes hemorrhages, swollen retinal veins, and edema or swelling. This often leads to visual loss.
If the occlusion is severe, there can also be marked ischemia or closure of the capillaries (small blood vessels). This can lead to abnormal blood vessels in the eye (neovascularisation), haemorrhage into the vitreous and even abnormal blood vessels in the front of the eye that can lead to high intraocular pressures and glaucoma (rubeosis).
It has been noted for forty years that some central vein occlusions are severe, leading to blindness and complications and others are less severe with some visual loss but maintenance of some vision. Those eyes with severe vein occlusion have blood vessel closure (ischemia) and are more likely to have problems.
Q: What is Branch Retinal Vein Occlusion (BRVO)?
A: A more localised blockage of the retinal venous system may occur and this is called a branch vein occlusion. The arteries and veins in the back of the eye cross each other like highways on a map. At the places where arteries cross veins, there can be a blockage of the vein. The artery and vein share a common sheath and as the artery thickens with age and hypertension, the vein can be blocked by the thickened artery.
Most patients who have this problem have risk factors for vascular disease. This may be diabetes, high blood pressure, arteriosclerosis, open angle glaucoma or a condition called thrombophilia. In younger patients, usually under age 40, we check for clotting disorders. Sometimes we find an important abnormality that needs to be treated. If there is a family history of strokes or miscarriages or if the patient has autoimmune problems, then the tests are particularly important. Since these problems are stroke-type events, we request that you check with your primary care doctor for a review of your medical condition.
These blockages may not have any symptoms if the occlusion does not involve the macula. If the macula is involved, then there can be swelling of the retinal tissue that can lead to visual loss (macular edema).
Laser treatment for BRVO has been shown to improve vision compared to the natural course without any treatment. The Lucentis study compared a control group that was treated like the vein occlusion study with a combination of untreated patients if the vision got better and laser treatment if the vision did not get better. In the Lucentis treated group, 61.1 % got better and in the control group (including laser) only 28.8 % improved three lines or more. The percentage of patients seeing 6/9 or better was 64.9 percent for the Lucentis group and 41.7 percent in the sham group. This difference, while significant was not large.
Because the Lucentis shots often require monthly injections, we usually treat with both approaches with the hope of being able to stop the monthly injections.
The most common systemic cause for BRVO is hypertension (blood pressure). It can also be seen in arteriosclerosis and diabetes. Sometimes there is no associated problem.
Q: What treatments are available for Retinal Vein Occlusions (RVOs)?
A: The treatment options are enlisted below
1. Treatment with Lucentis
There is a new treatment that is effective in improving vision and clearing macular edema in central retinal vein occlusion. It is injection of Lucentis into the eye once a month for at least six months. Lucentis is an antibody against the molecule that causes macular edema and the growth of abnormal vessels (Vascular Endothelial Growth Factor or VEGF)
Vision improvement is rapid and seen on average, by seven days. Patients were treated with six monthly injections. After six months it may be possible to stop the treatment, but this varies from patient to patient. If the vision is down, we usually restart treatment immediately. If vision is good and there is no macular edema, observation may be continued.
In CRVO, about 50 % of the patients got significantly better (3 lines improvement in vision) compared to 17 % in people who underwent no treatment.
In BRVO, about 60 % patients improved by at least three lines compared to 30 % of patients who underwent laser only
2. Treatment with Avastin
This is another Anti –VEGF drug, which is FDA approved for treatment of cancers and has also been shown to work for macular edema. Research has proven it to be equally effective and safe as Lucentis.
We prefer to use Lucentis when possible and patient permitting, because it is the drug that has been shown to work in large clinical trials and is prepared under strict and specific FDA guidelines for use inside the eye.
3. Treatment with Steroids
Intraocular steroid injections like triamcinolone (IVTA) and Ozurdex are another treatment option. The SCORE trial was a large multicentre trial that showed a benefit in CRVO but not in BRVO.
The duration of action is much longer and so the need for less frequent injections. In some cases like recurrences or long standing vein occlusions, they are more effective than anti-VEGF injections.
However there is a significantly higher risk of glaucoma and cataracts in patients given steroid injections, especially if they are repeated.
Ozurdex is a long acting steroid implant, which contains a different steroid, dexamethasone. The duration of action is for about 4 months. The risk of cataract and glaucoma is marginally less than triamcinolone (IVTA).
While Lucentis is a better, safer option for most cases, sometimes steroid treatment by itself or in combination with Lucentis may be warranted.
4. Treatment with Laser
In two large, multicentre clinical trials conducted in the 1990’s (the Central Vein Occlusion Study, or CVOS and the Collaborative Branch Vein Occlusion Study, or BVOS) demonstrated that laser treatment to the macula (center of vision) demonstrated a benefit in BRVO but not in CRVO.
However, laser treatment outside the macula (peripheral or scatter laser) was demonstrated to be effective when abnormal blood vessels grow in the retina or iris (neovascularisation). This is a rare but serious complication that can result in bleeding inside the eye (vitreous haemorrhage) and increased eye pressure (neovascular glaucoma).
Recent evidence shows the benefit of scatter laser in long term reduction of VEGF levels and indirectly reducing macular edema in all vein occlusions.
Q: What are occlusions of the retinal and optic nerve arterioles?
A:
1. Central Retinal Artery Occlusion
The arterial circulation of the eye can become occluded just like the venous system. What you see inside the eye is completely different. In a vein occlusion there is edema and haemorrhage. In retinal artery occlusion, the retina turns white.
Patients with central retinal artery occlusion lose vision suddenly. Unfortunately, the visual loss in central retinal artery occlusion is usually irreversible, although there may be some improvement over time.
There is no good treatment of central retinal artery occlusion. Lowering the eye pressure by drugs, paracentesis or ocular massage or breathing into a bag have been suggested, but they don’t seem to help.
Treating the artery occlusion aggressively like you would treat a stroke in the brain with TPA (tissue plasminogen activator) has also been tried, but without success.
If you have a central retinal artery occlusion, it is important to figure out why.
Sometimes these problems are caused by emboli (small piece of cholesterol or other matter) from the heart or the carotid artery. Sometimes the blockage is a thrombus (clot) that forms in the artery itself with an aggregation of platelets. Patients with artery occlusion need to be checked by their doctor and usually have a carotid ultrasound to rule out disease there and an echo cardiogram to rule out a clot in the heart. In younger patients there may be a heart condition called foramen ovale where there is a hole between the right heart and the left heart and emboli can cross into the arterial circulation. Patients also need to control their cholesterol and high blood pressure if elevated. Usually such patients are treated with aspirin or clopilet.
2. Branch Retinal Artery Occlusion
Like in vein occlusions, sometimes only a part of retina is involved and this is a branch retinal artery occlusion. The same risk factors related to central artery occlusions also apply to branch artery occlusions. Medical evaluation should be undertaken.
There is a unique subset of retinal emboli where the ophthalmologist can actually see flecks of cholesterol in the eye. Sometimes they block the artery and sometimes not. Patients with plaques in the retina called Hollenhorst plaques need to be evaluated to rule out carotid disease and hypercholesterolemia.
3. Ischemic Optic Neuropathy
It is the occlusion of the choroidal vessels around the optic nerve. This can lead to sudden visual loss and usually affects the upper or lower field of vision. There are currently no proven treatments although steroids and anti-VEGF drus like Lucentis have been tried with mixed results.
Ischemic optic neuropathy may be caused by hypertension or arteriosclerosis. It is also associated with temporal arteritis, an inflammatory disease of the arteries of the head. Additional symptoms with temporal arteritis are headaches. Difficulty chewing, feeling tired, difficulty getting hands above the head, scalp tenderness and weight loss. Patients suspected of this condition need blood tests, ESR and c-reactive protein. Often a biopsy of their temporal artery is needed to confirm the diagnosis. The treatment for temporal arteritis is high dose steroids so it is important to be sure of the diagnosis if treatment is going to be continued for a long time.
Ischemic optic neuritis has also been associated with drugs to treat erectile dysfunction like Viagra. If you are taking these drugs it is important to stop and be evaluated.